 |
|
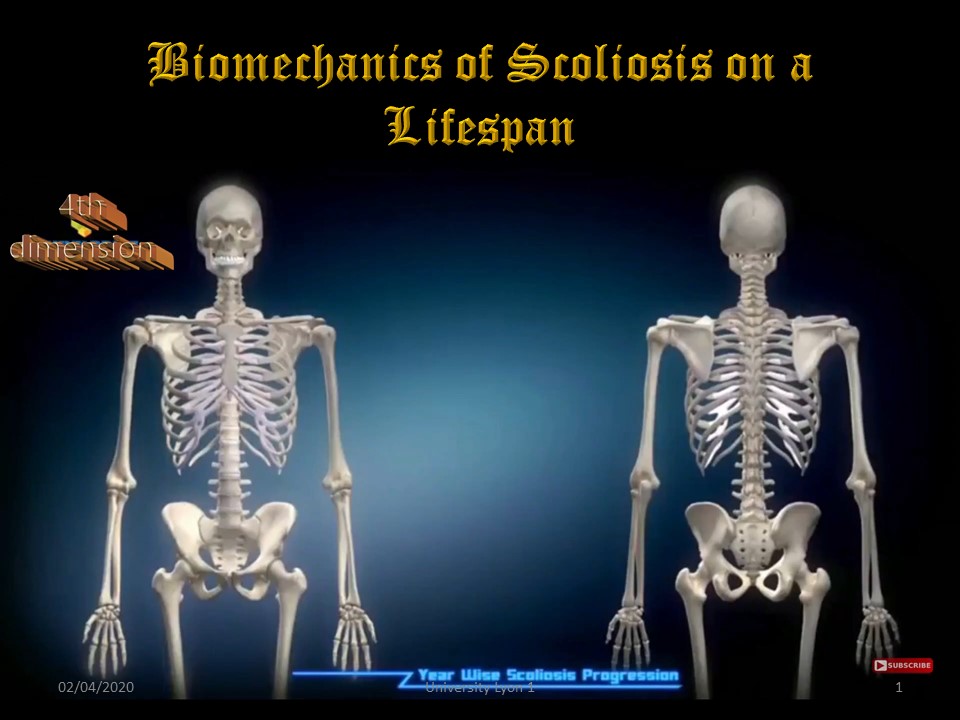 |
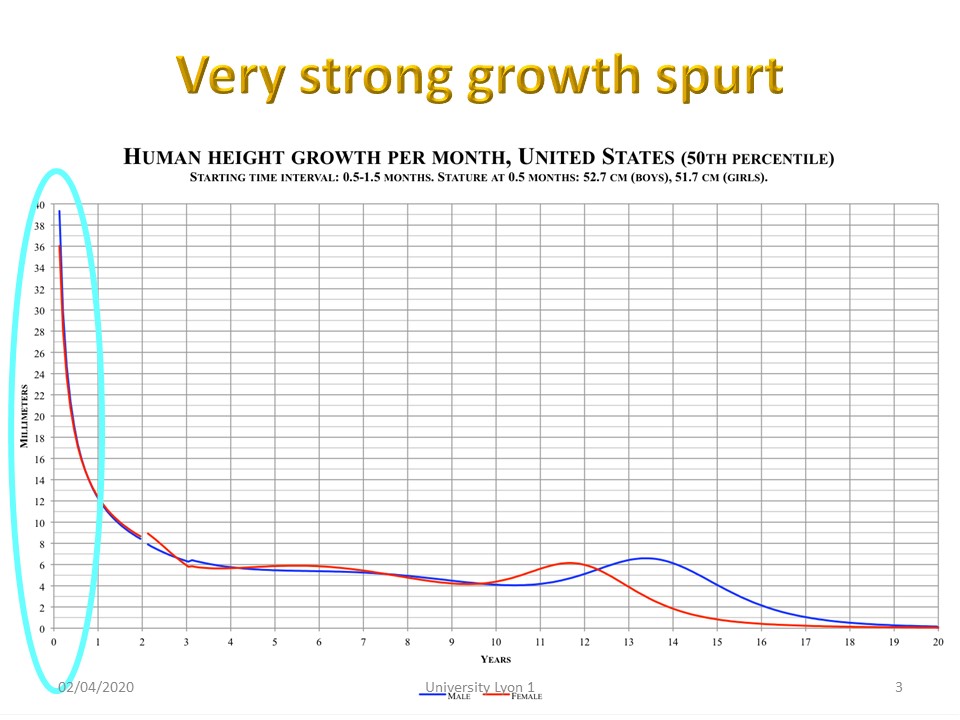
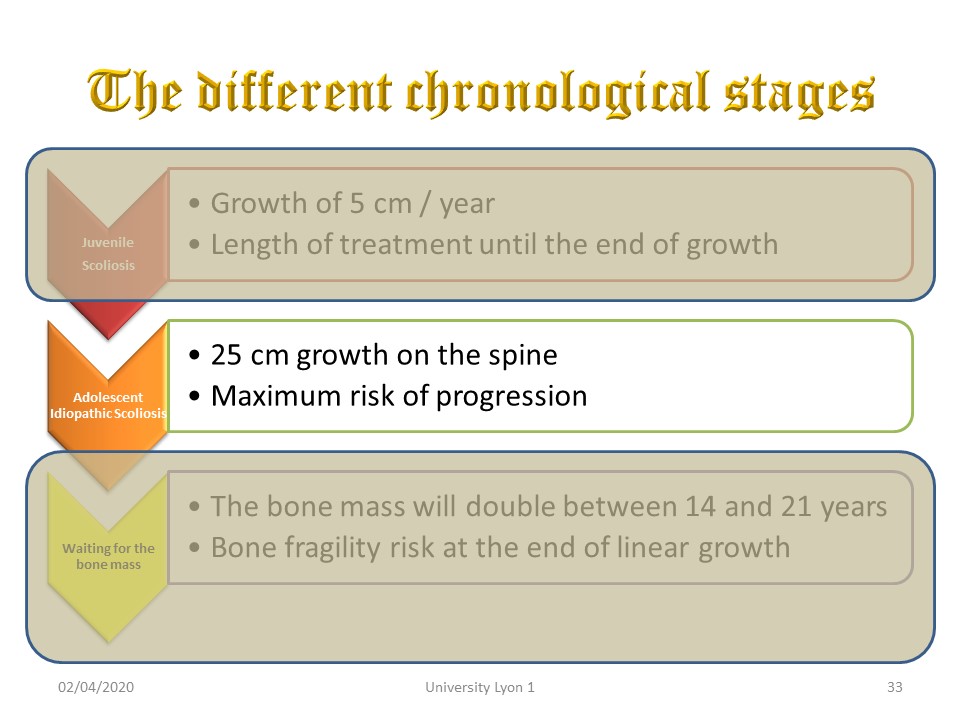
Scoliosis evolves throughout life, which is its fourth dimension. It has particular biomechanical characteristics at each stage.
|
 |
|
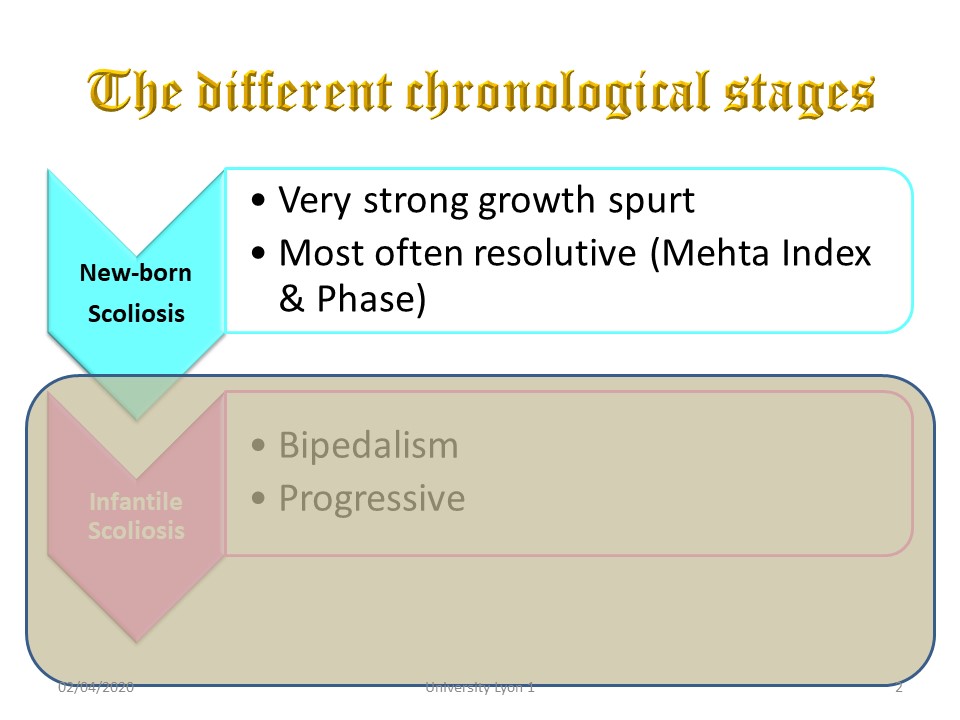 |
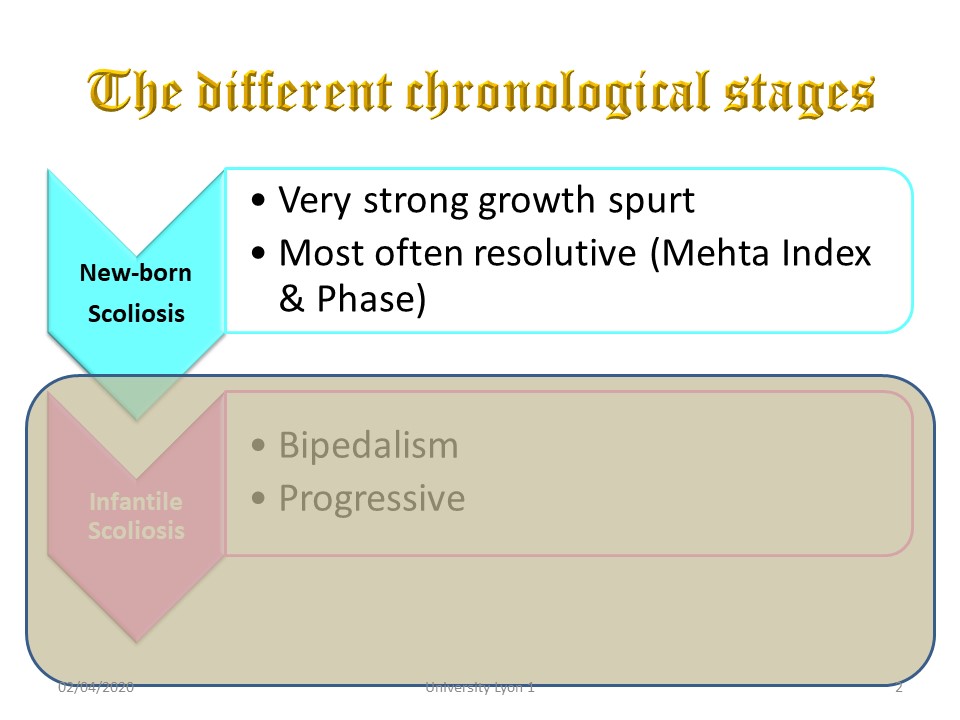
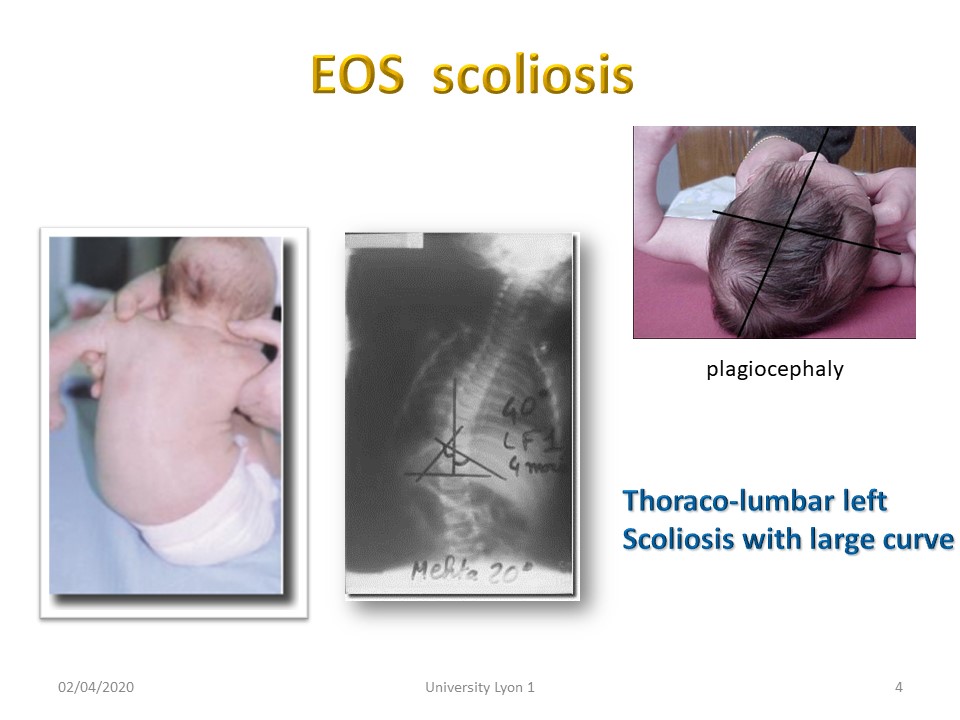
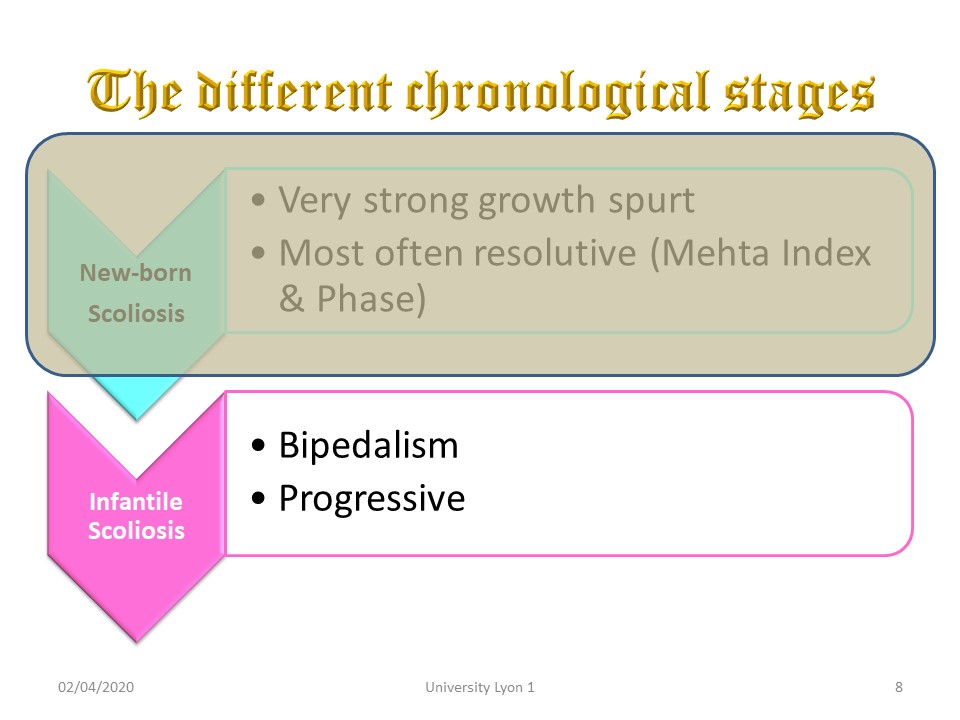
The first stage is new-born scoliosis. The growth is very important. These scoliosis are most often related to asymmetrical posture.
|
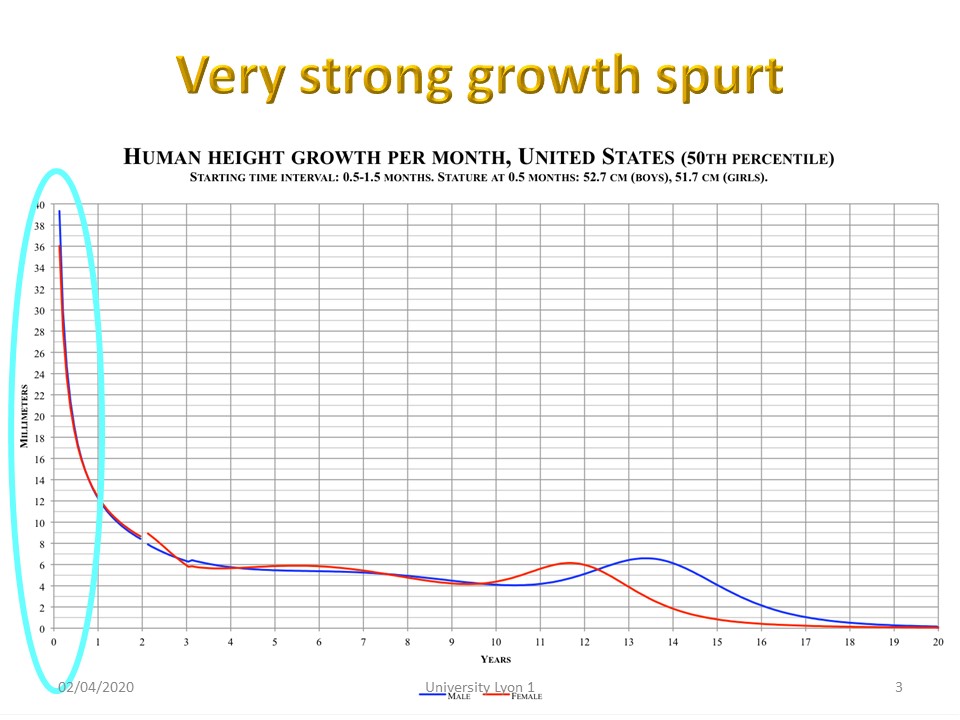 |
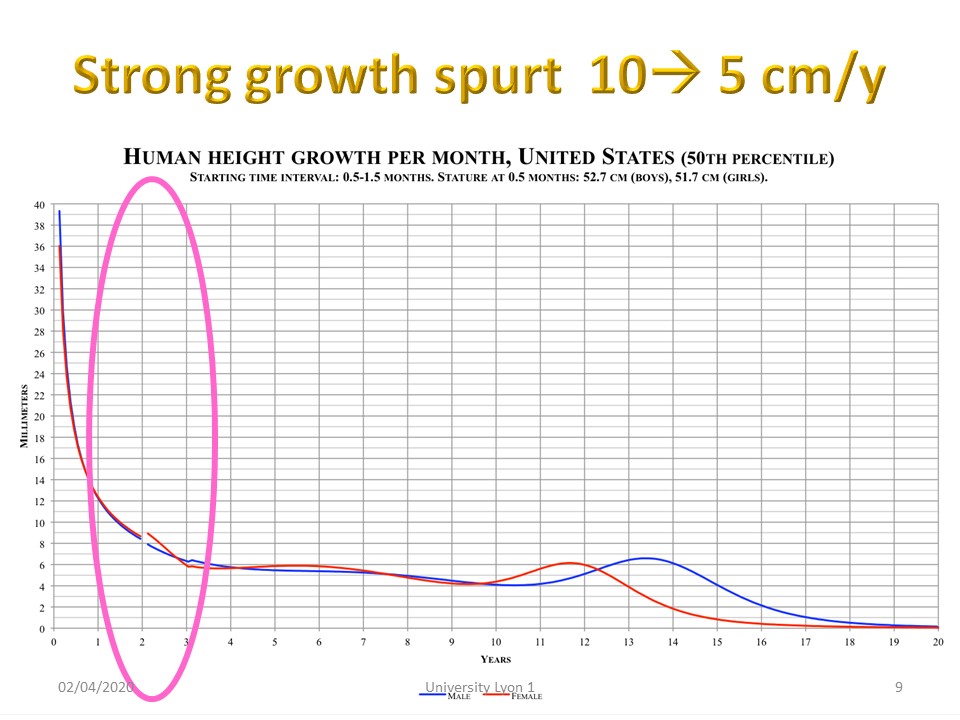
Rapid growth will decrease gradually during the first year of life.
|
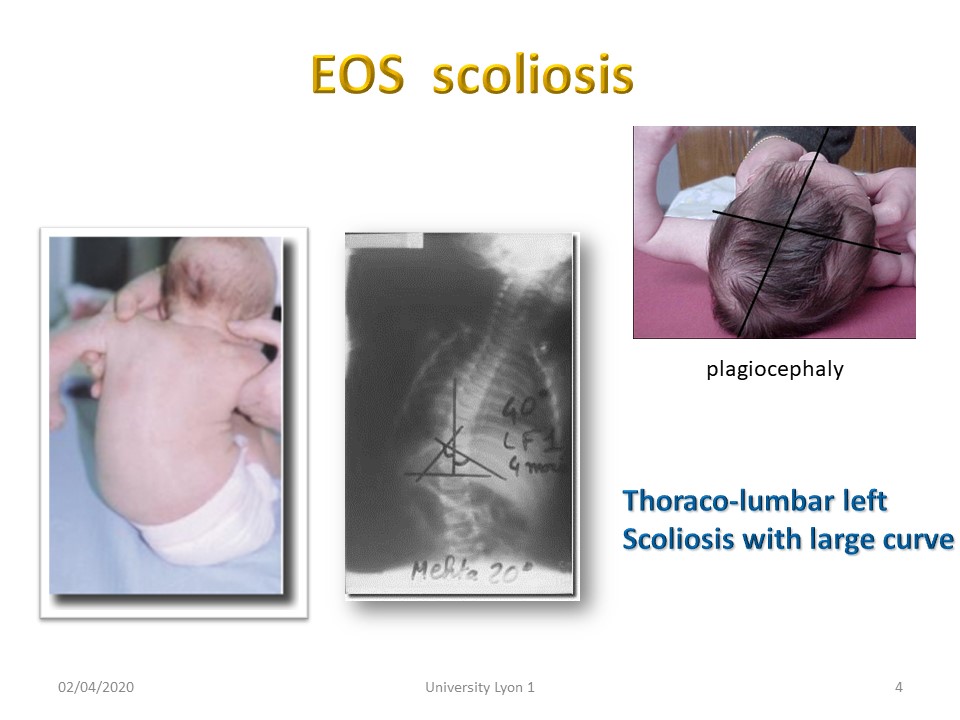 |
Scoliosis at this age have a large thoraco-lumbar curvature. Asymmetry extends to the skull with plagiocephaly. Scoliosis is lateralized 50% are on the left and 50% on the right. These are the only scoliosis for which it is possible to predict progression.
|
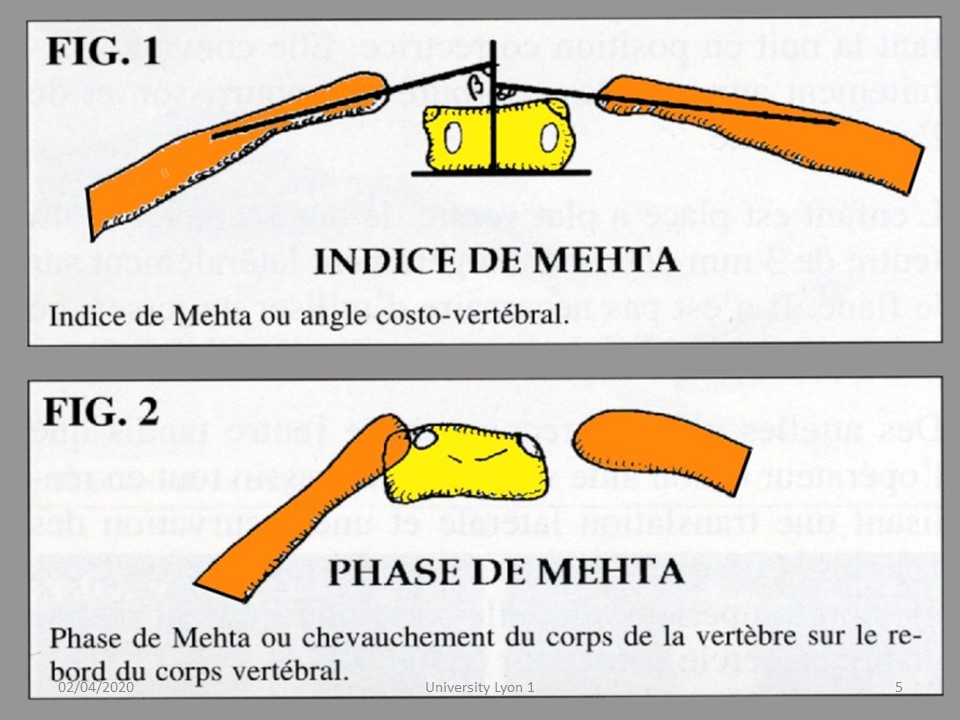 |
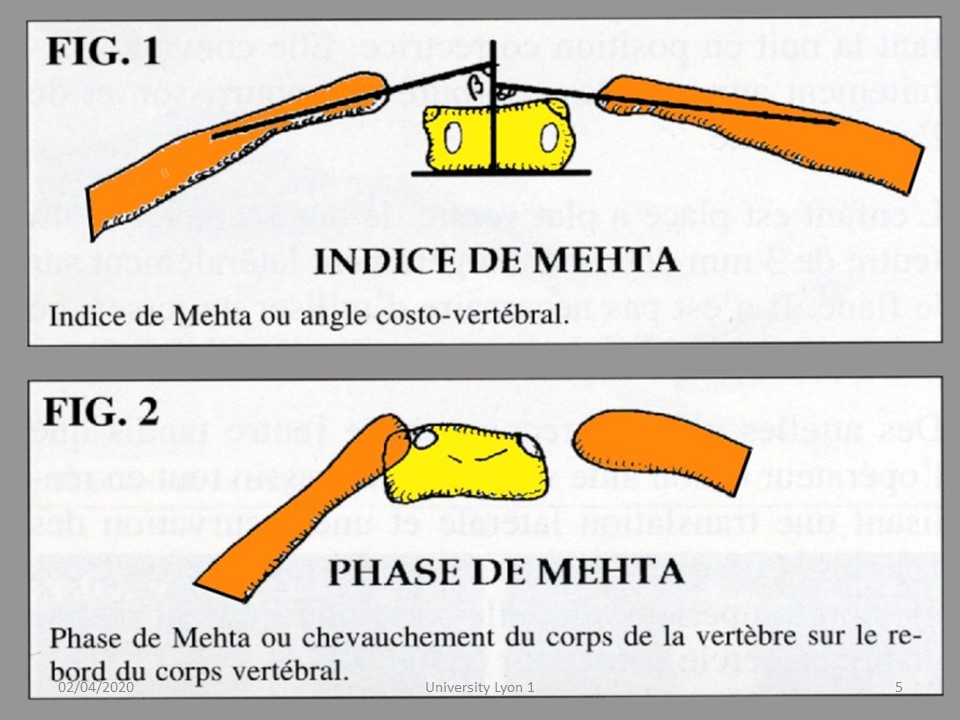
The Mehta index or costo-vertebral angle is measured at the level of the horizontal vertebra at the apex of the curvature. When the difference between the 2 angles is greater than 20 °, it is a progressive scoliosis. Similarly, when the tip of the convex rib overlaps the vertebral body, scoliosis is progressive. These 2 radiological signs allow an early treatment while avoiding the over-treatment.
|
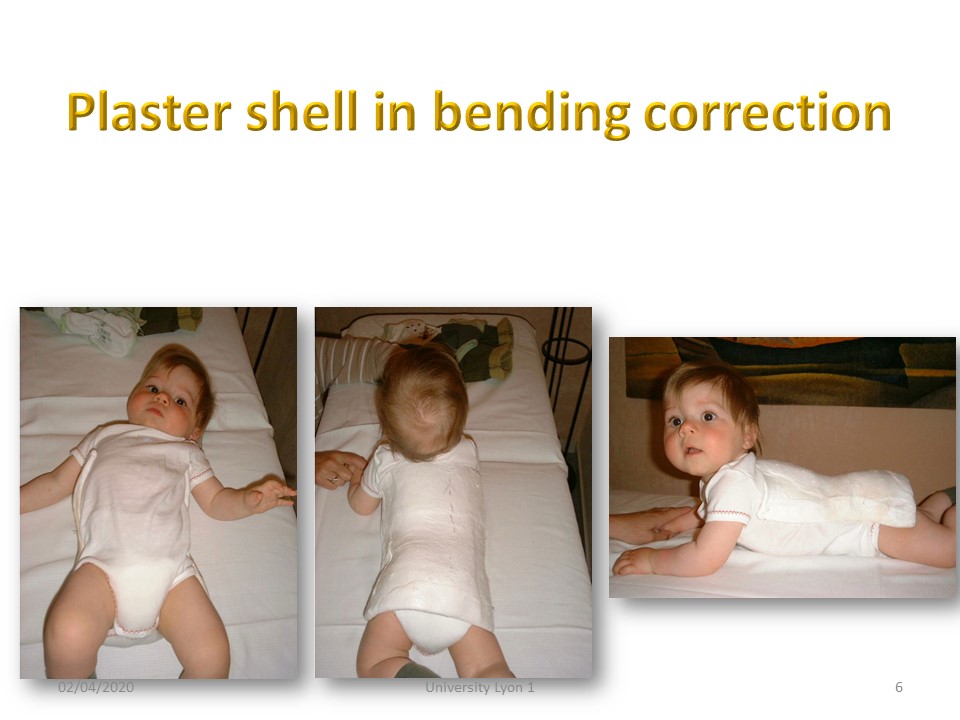 |
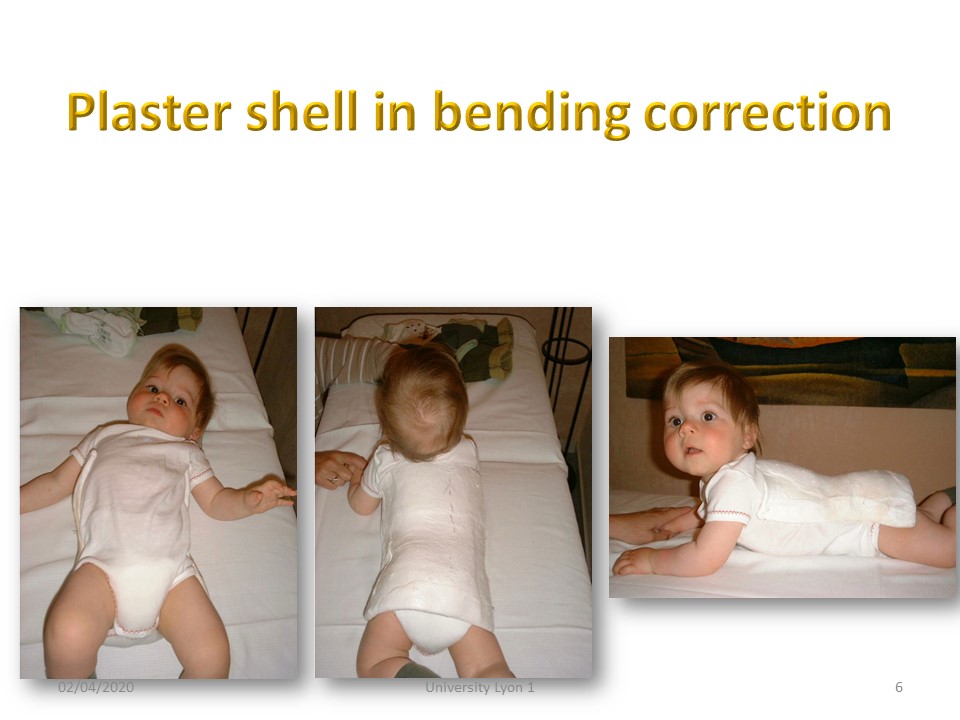
When the prognosis is progressive, the treatment consists in the realization of a posterior plaster cast shell in corrective bending of the scoliosis.
|
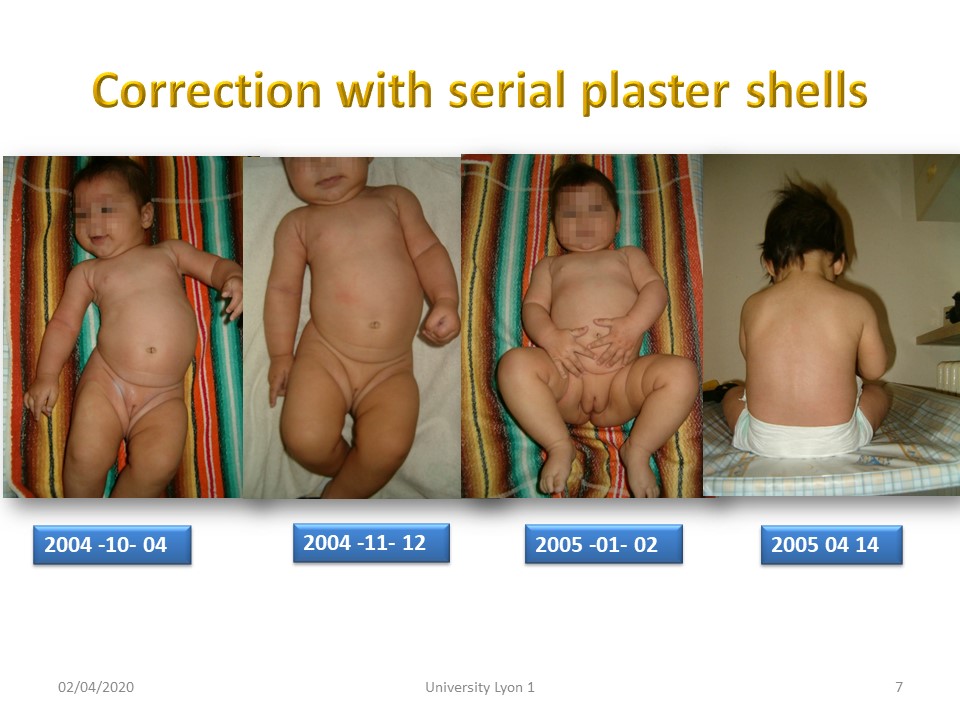 |
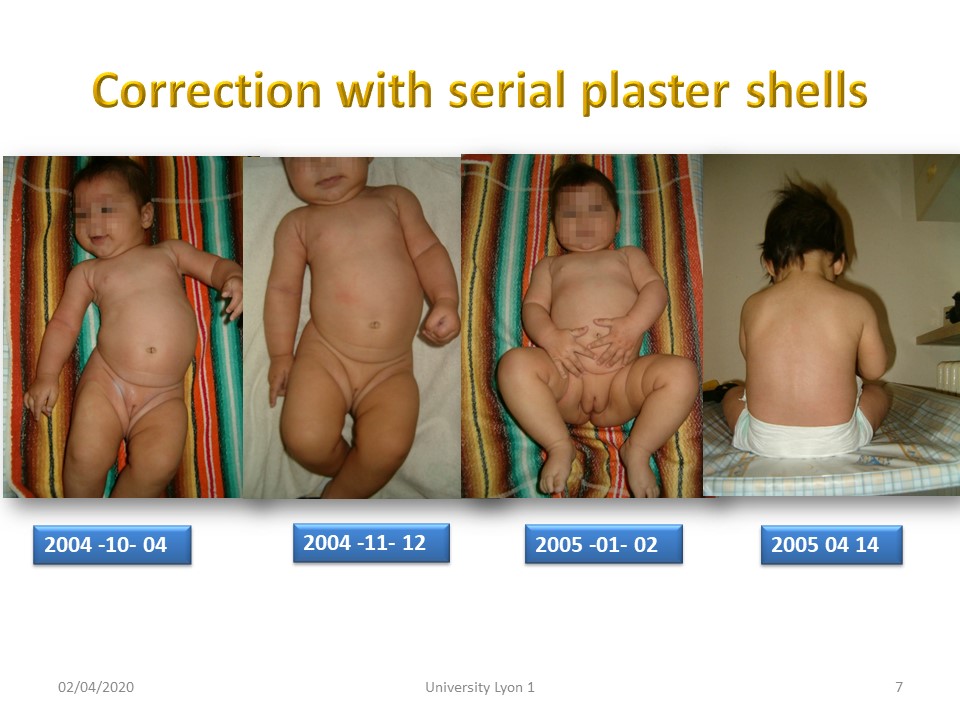
Here is an example of progressive correction of scoliosis in 6 months.
|
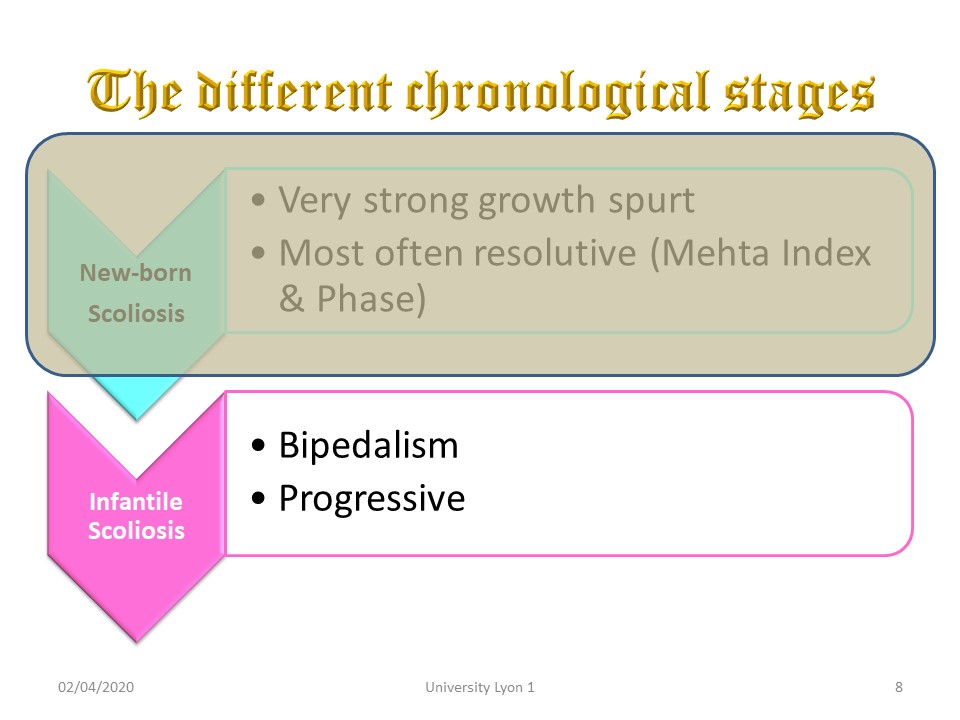 |
From 1 year to 3 years, the child will walk. The evolution of these scoliosis is biomechanically linked to an imperfect and immature verticality. The realization of braces is difficult.
|
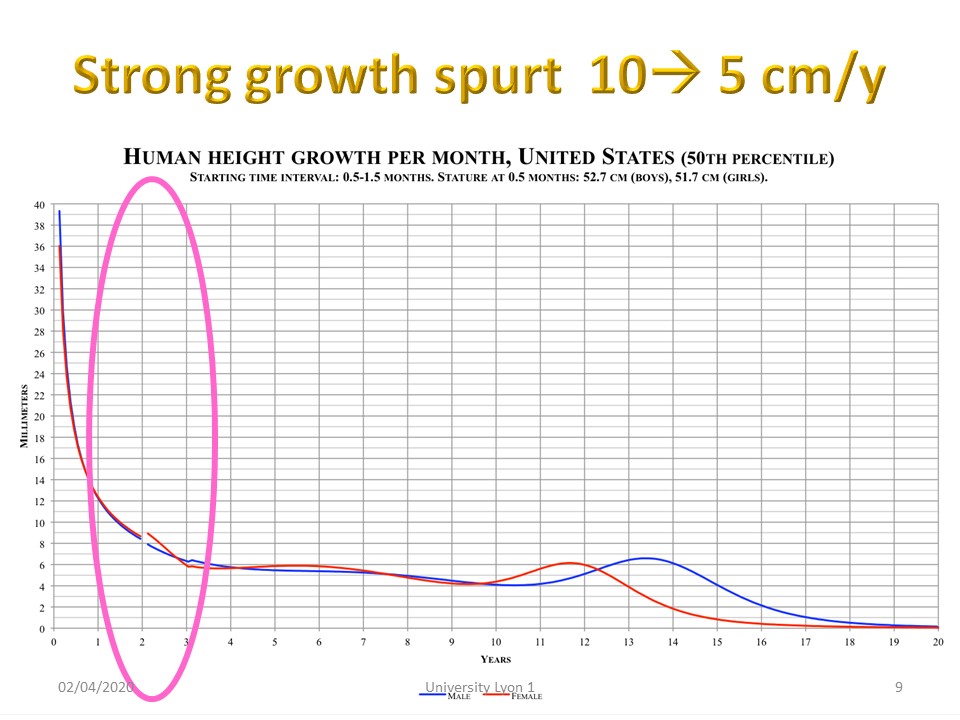 |
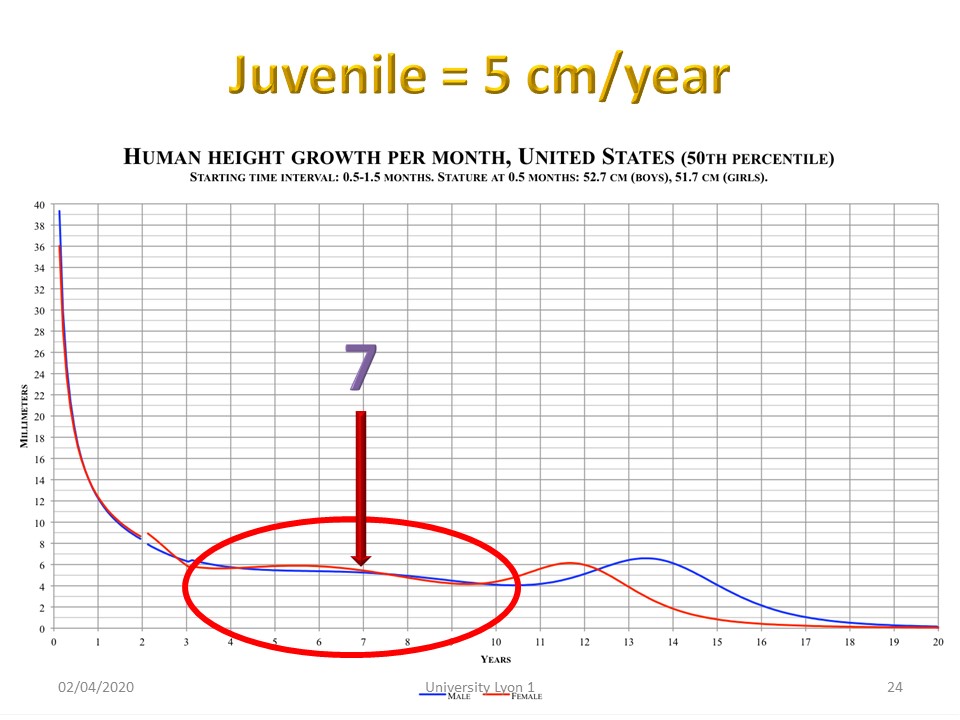
Stature growth remains significant from 10 to 5 cm per year at the age of 3 years.
|
 |
It is especially a fundamental period for the development of the lungs and braces must not favour a restrictive syndrome.
|
 |
Plaster casts have a large front opening. Like clubfoot, the serial casting allows to gradually reduce scoliosis.
|
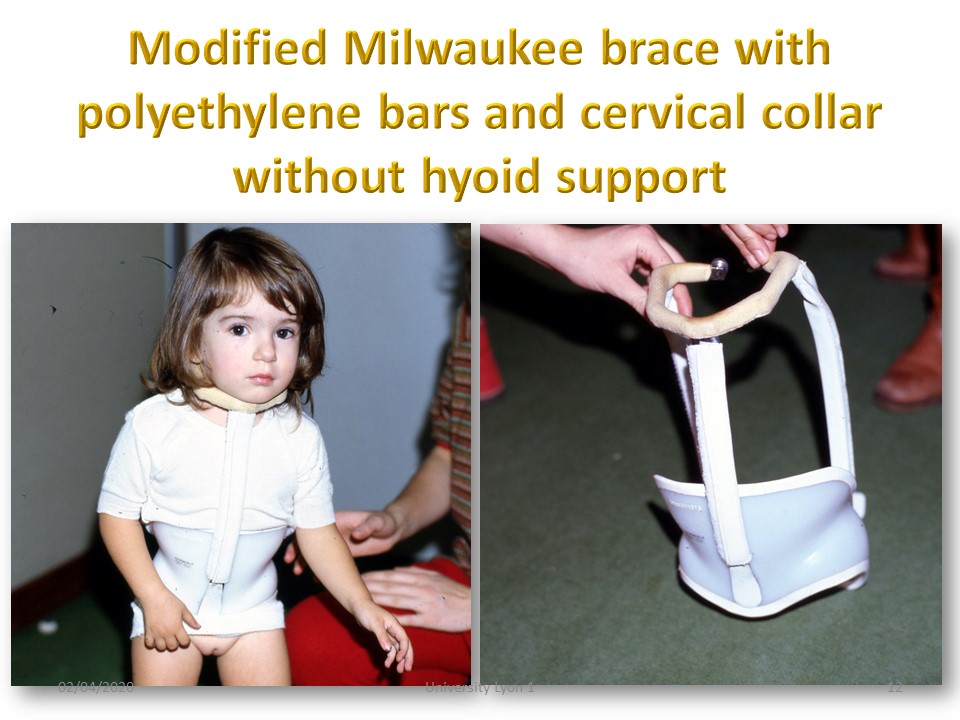 |
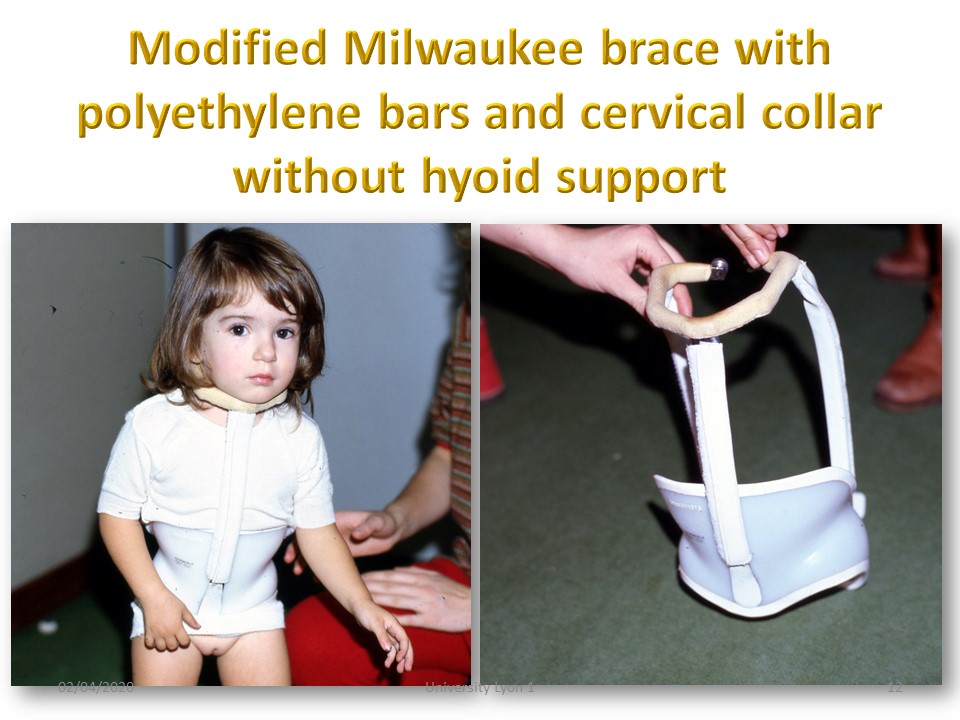
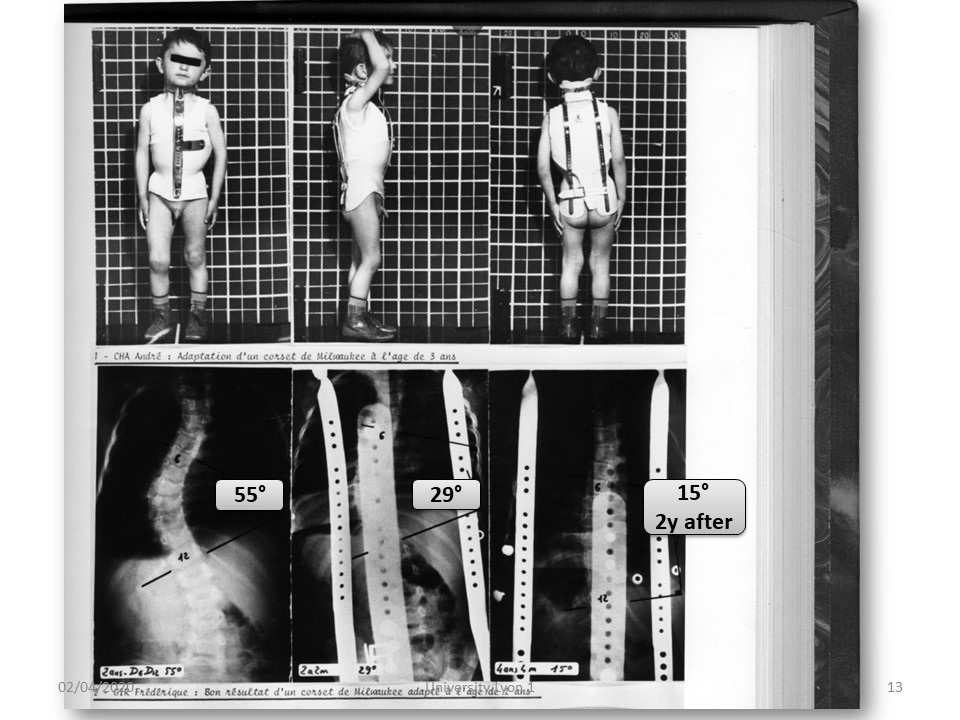
The Milwaukee brace should be adapted with use of polyethylene bars and a collar without hyoid support To avoid injury to the child, in case of a fall.
|
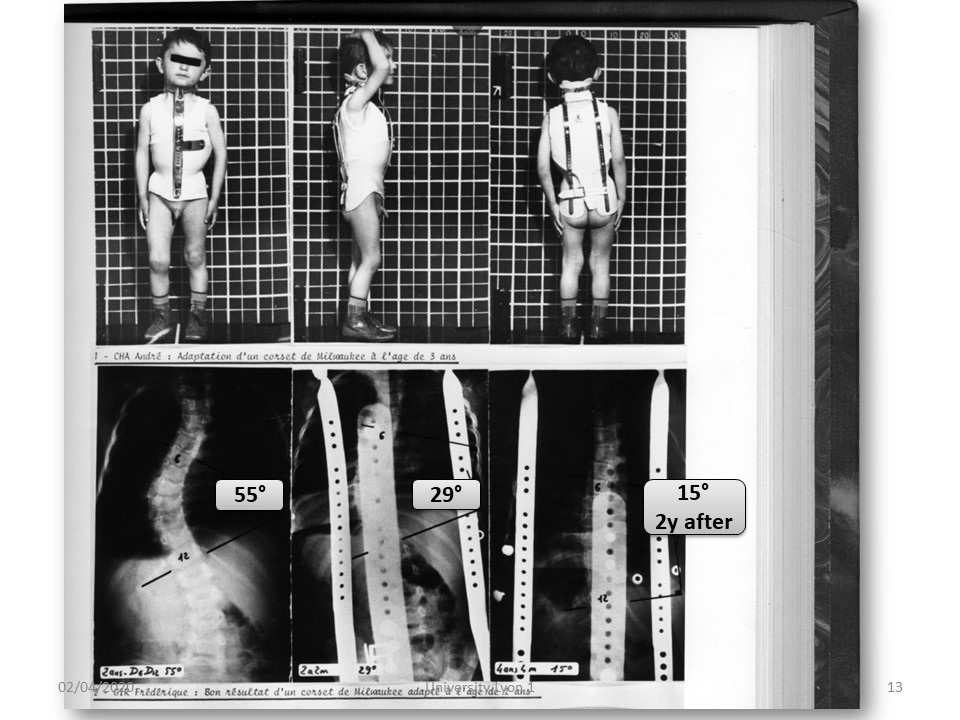 |
At this age the Milwaukee brace with translation along the vertical axis can effectively correct scoliosis.
|
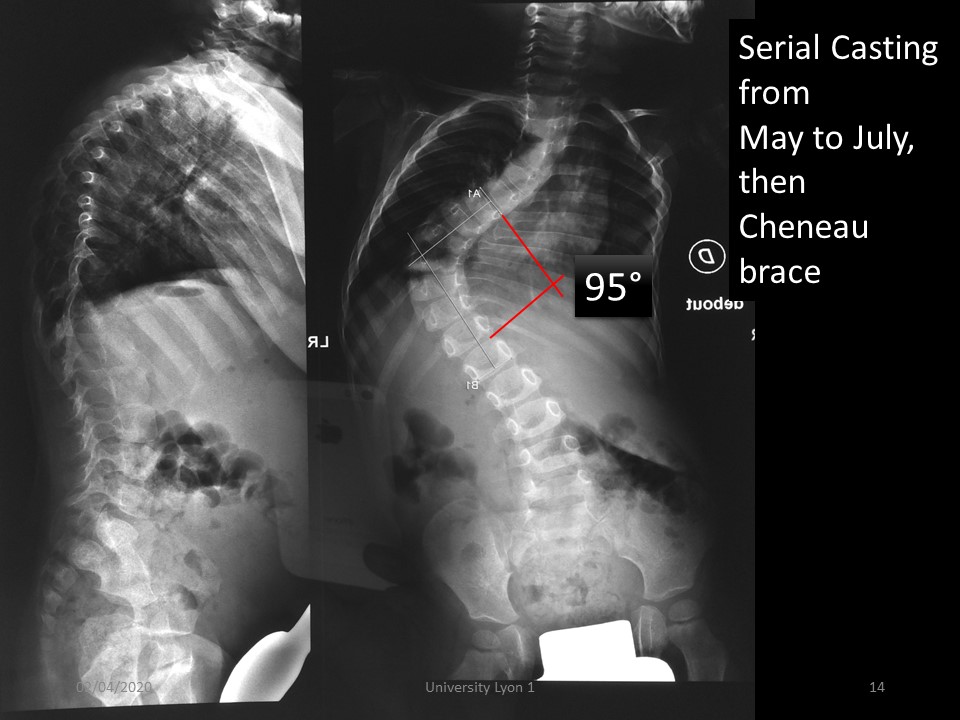 |
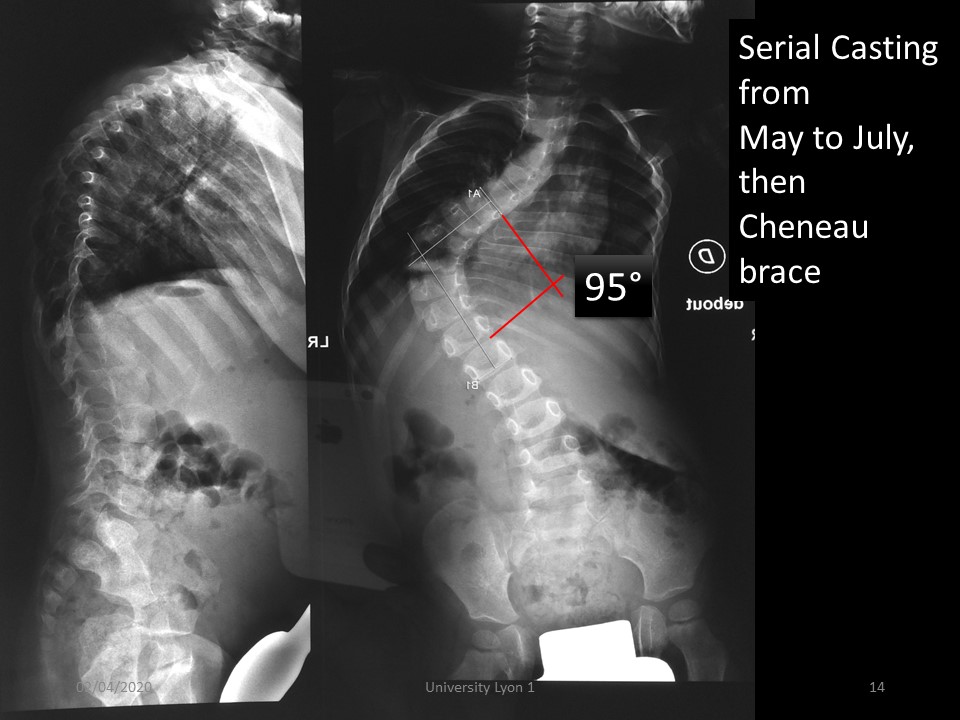
Sometimes after the serial casting, it is often too early to consider surgery. In this child a corset Chêneau has been made.
|
 |
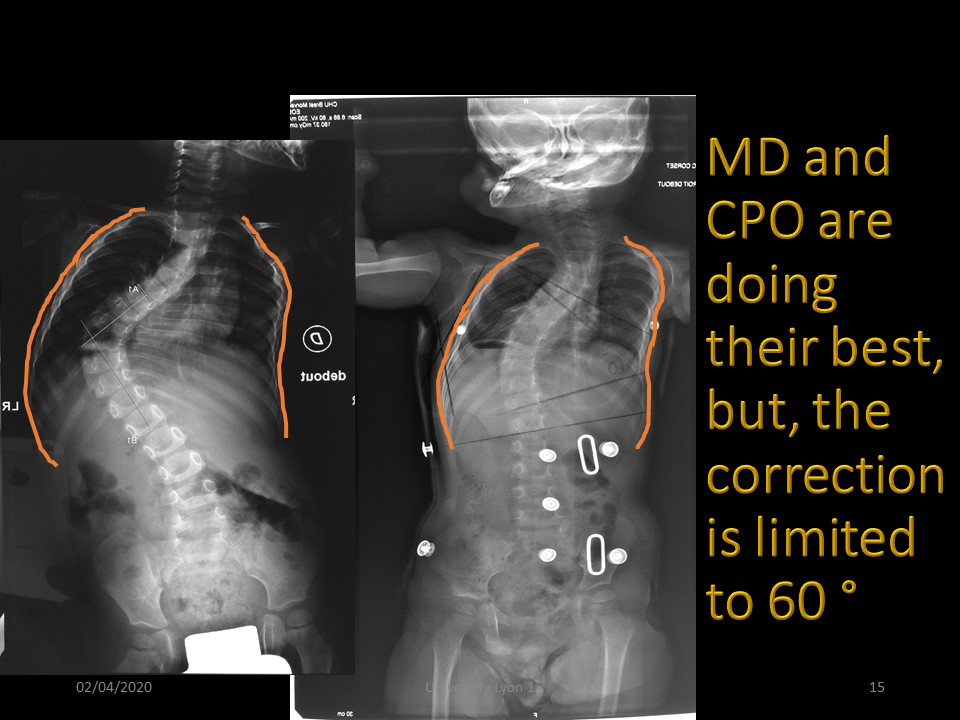
But the Chêneau brace realized did not maintain the high thoracic curvature and especially was not tolerated by the child
|
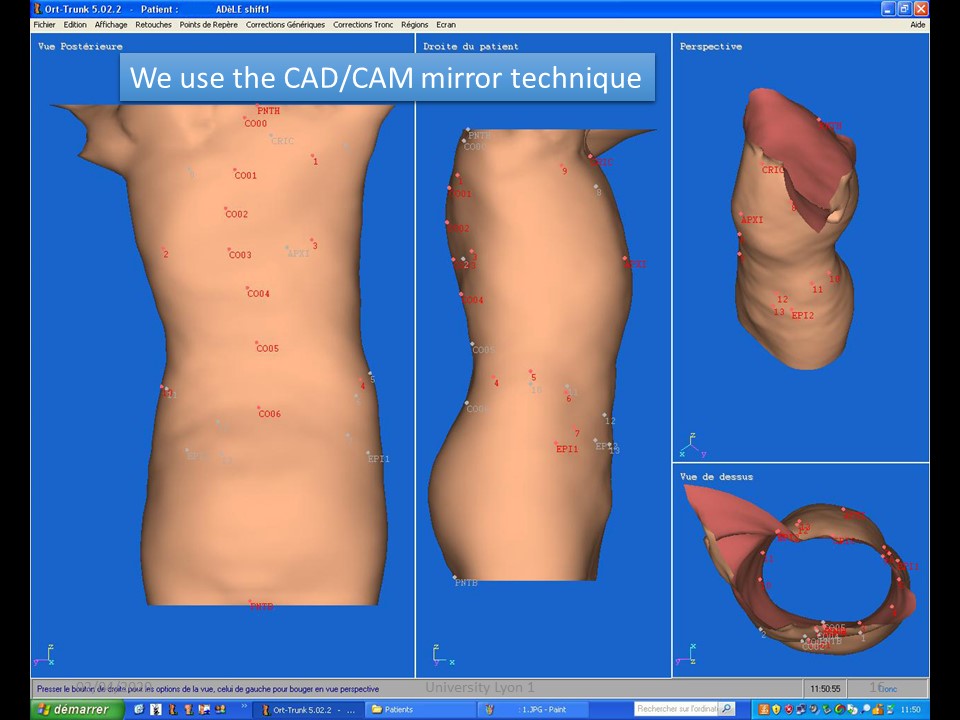 |
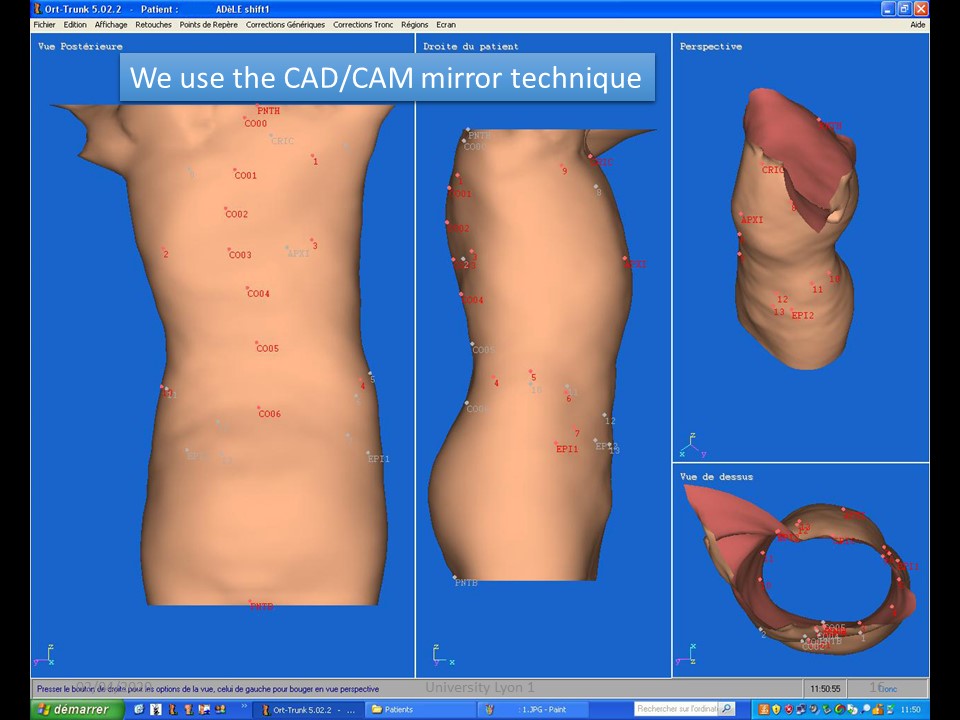
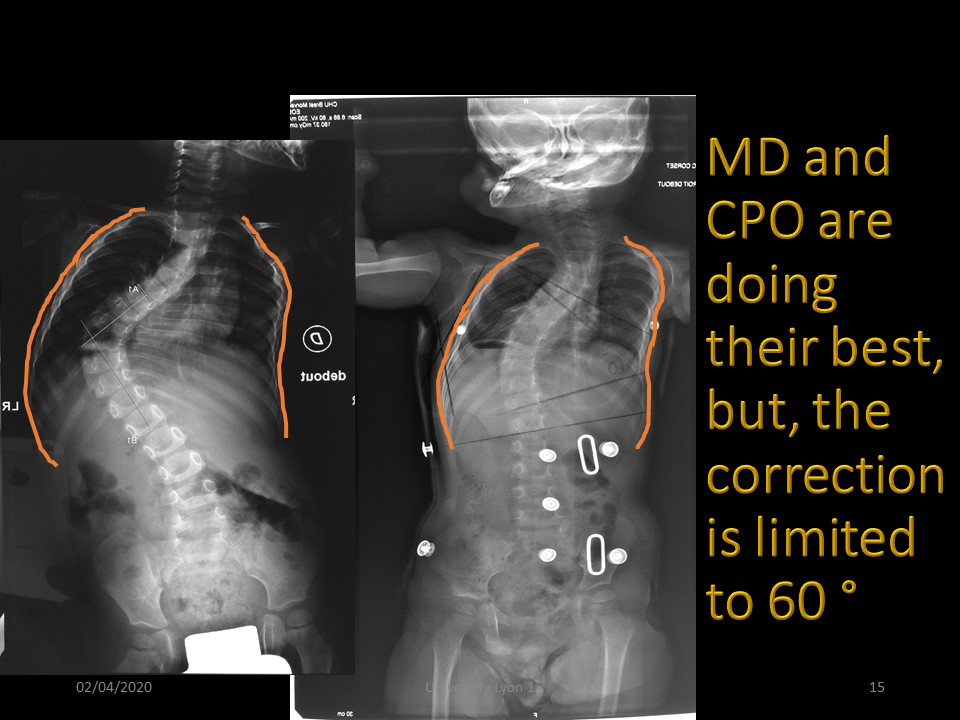
Mom wishing to try the new Lyon ARTbrace, a mirror CAD/CAM is done. The child is stretched to the maximum while standing. Only one scan is done and the positive is achieved by reversing right and left.
|
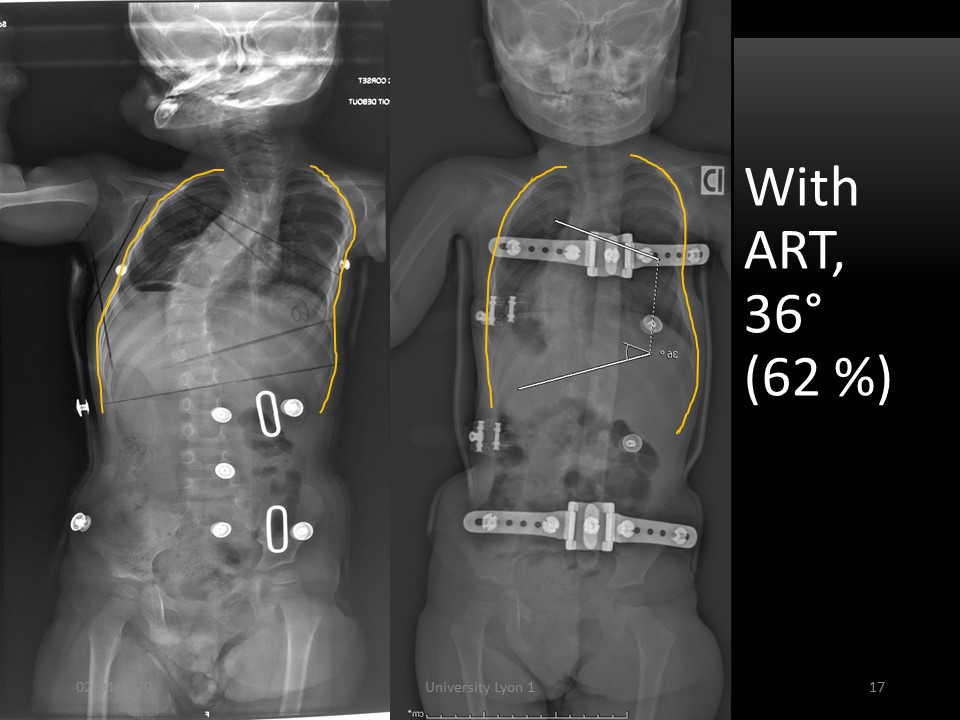 |
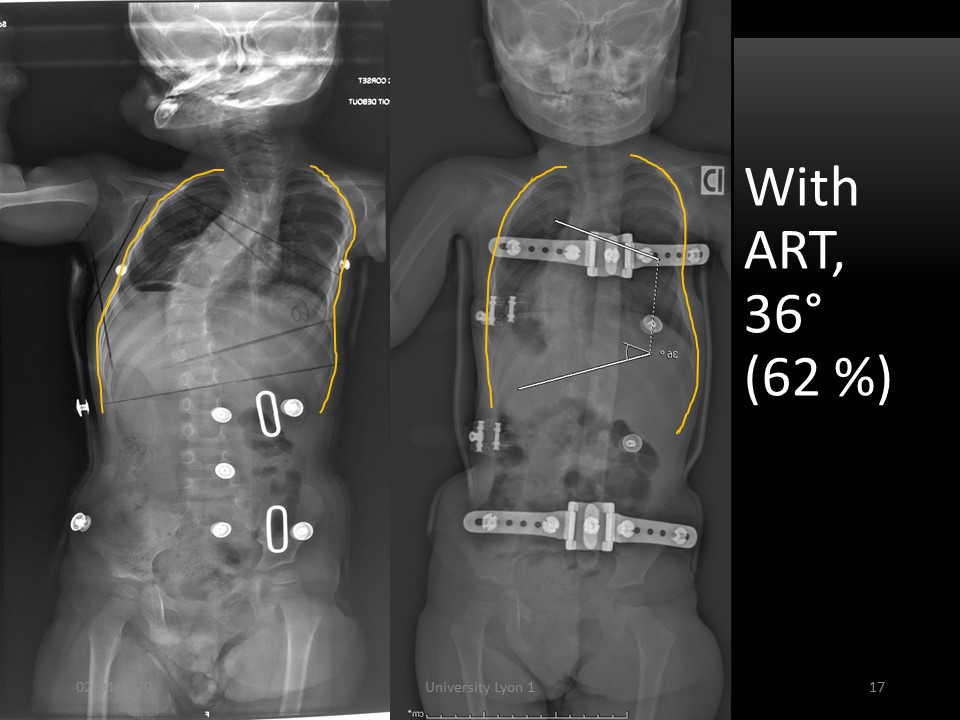
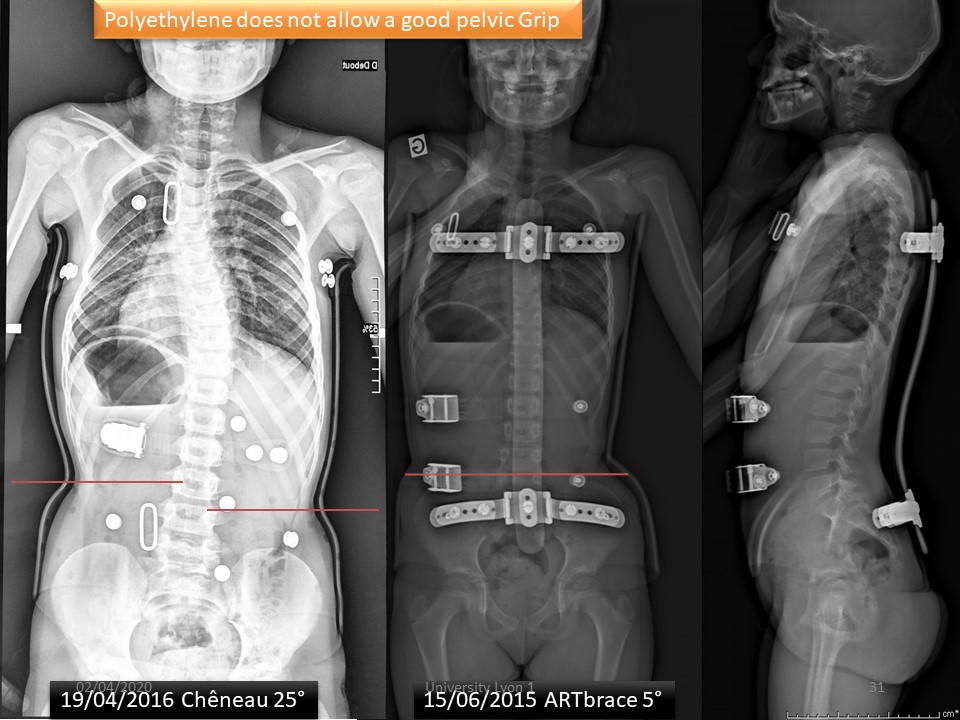
The comparison with the Chêneau is favorable with better maintenance of the thoracic cage at the upper part and improvement of the angular correction.
|
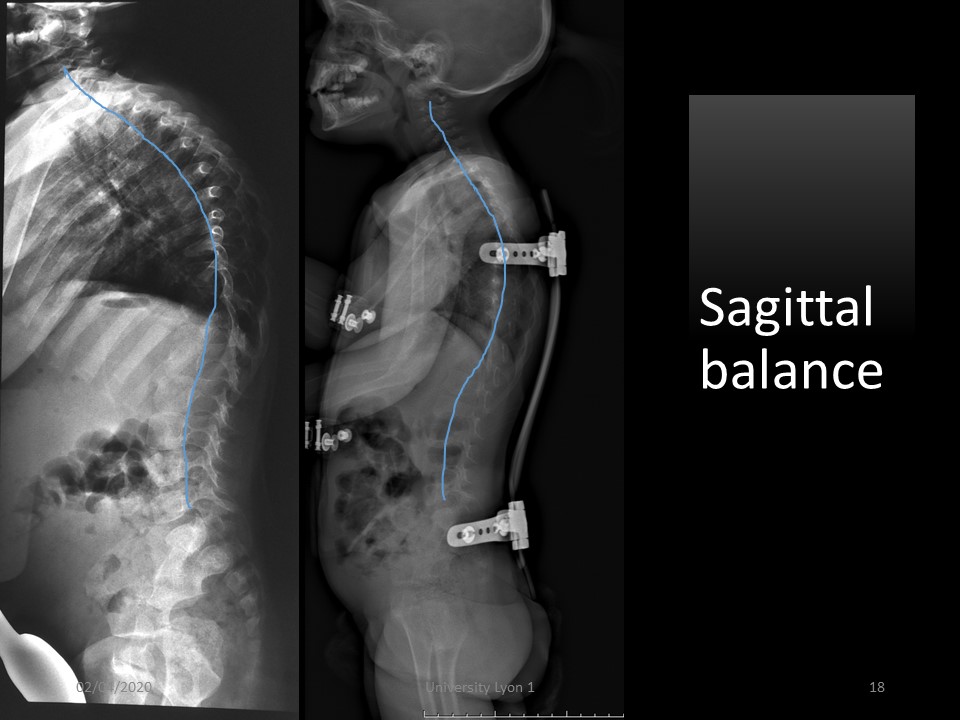 |
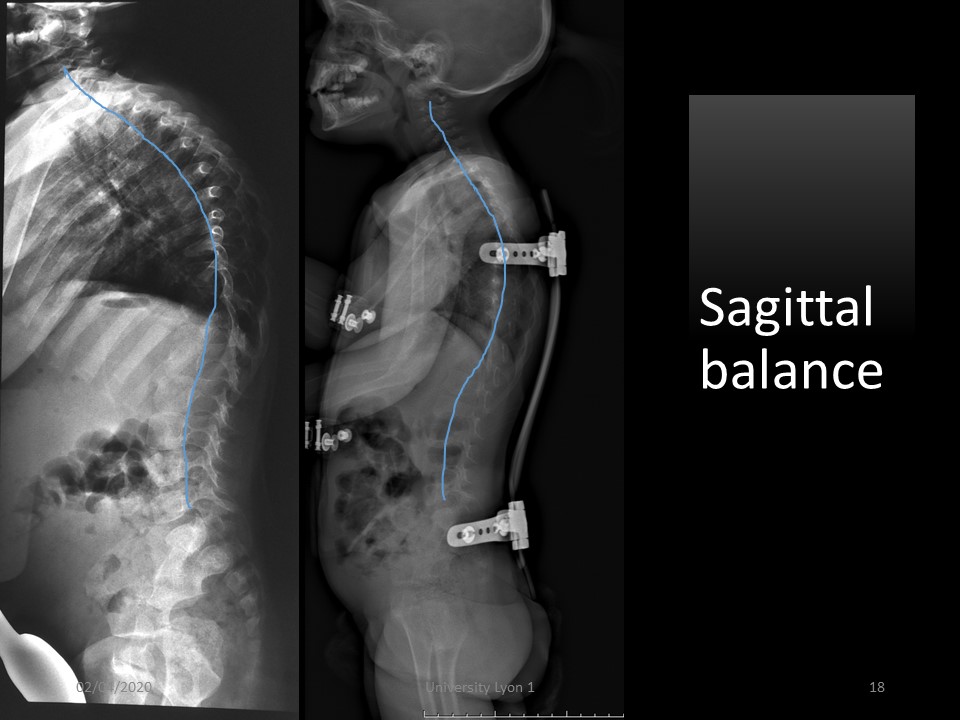
In the sagittal plane, the balance is also better.
|
 |
Clinical aspect in ARTbrace with polycarbonate of 3 mm. The day after the fitting the child goes tobogganing. At the last control the angulation was stable at 58 ° without brace. A large anterior thoracic expansion is performed to complete the expansion of the concavity.
|
 |
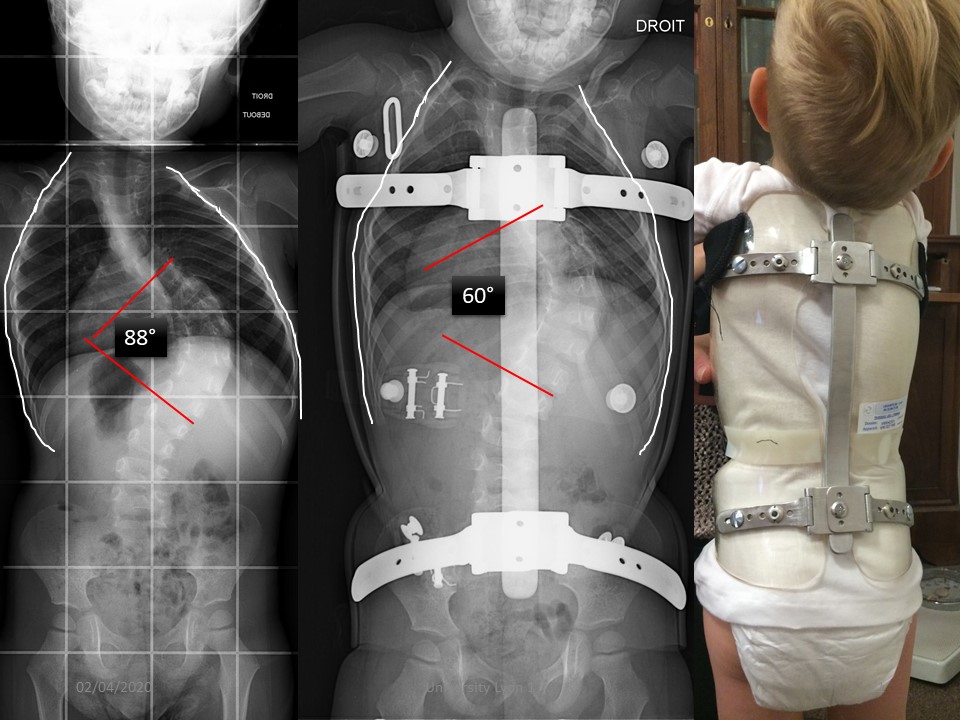
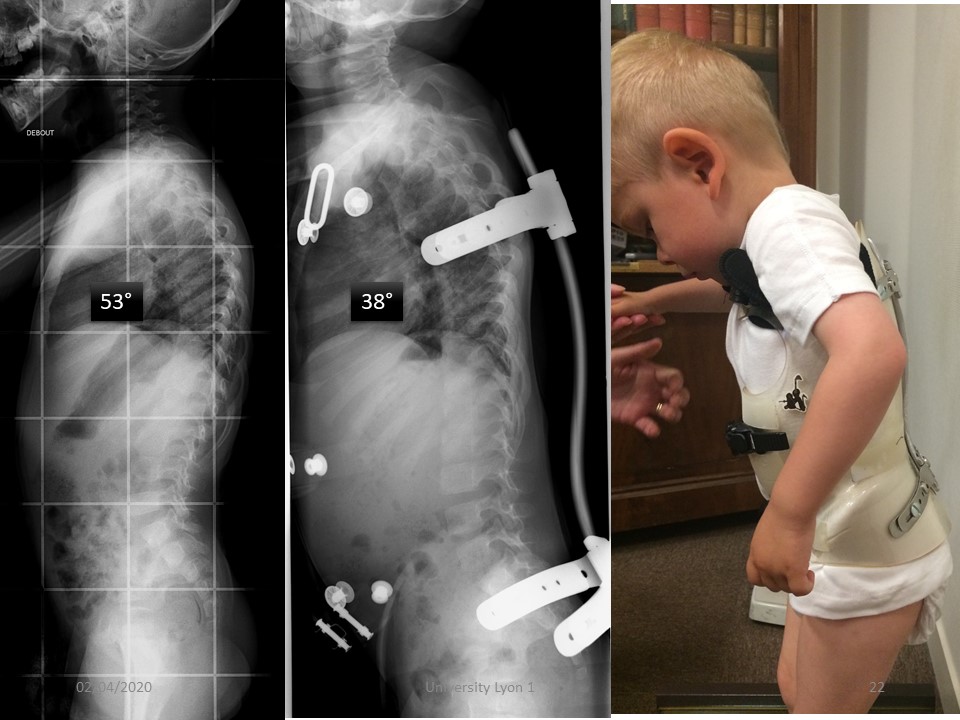
Leo's scoliosis is also an infantile scoliosis. The serial casting did not allow the stabilization of the scoliosis. He does not support the polyethylene brace made. We see him for the first time at the age of 2 1/2 years.
|
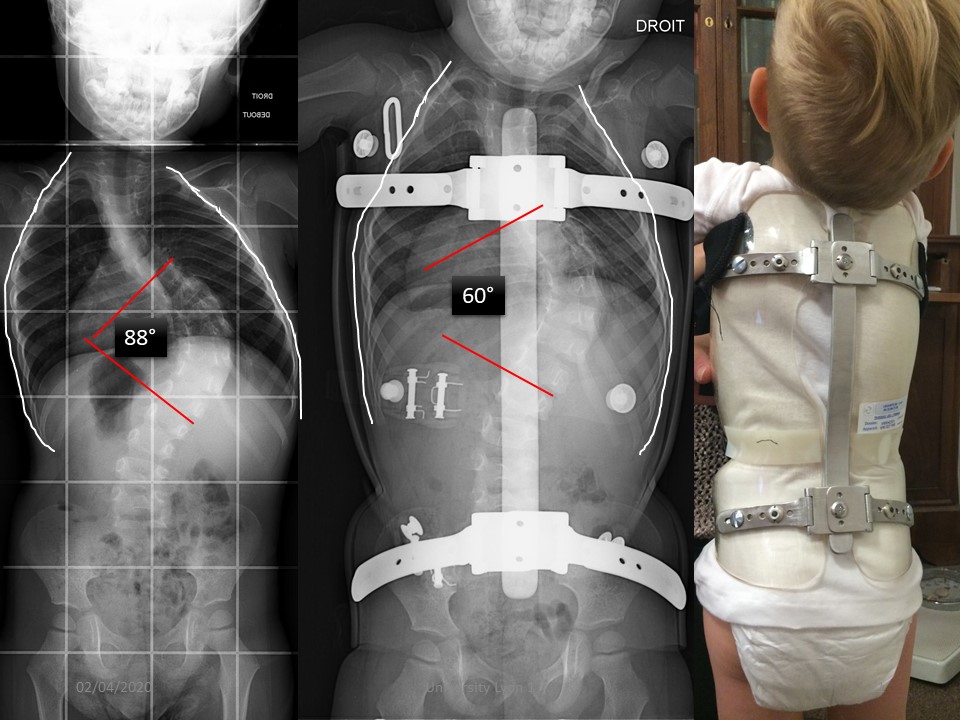 |
The brace is made using the mirror technique. The balance is correct, but the scoliosis is already very stiff.
|
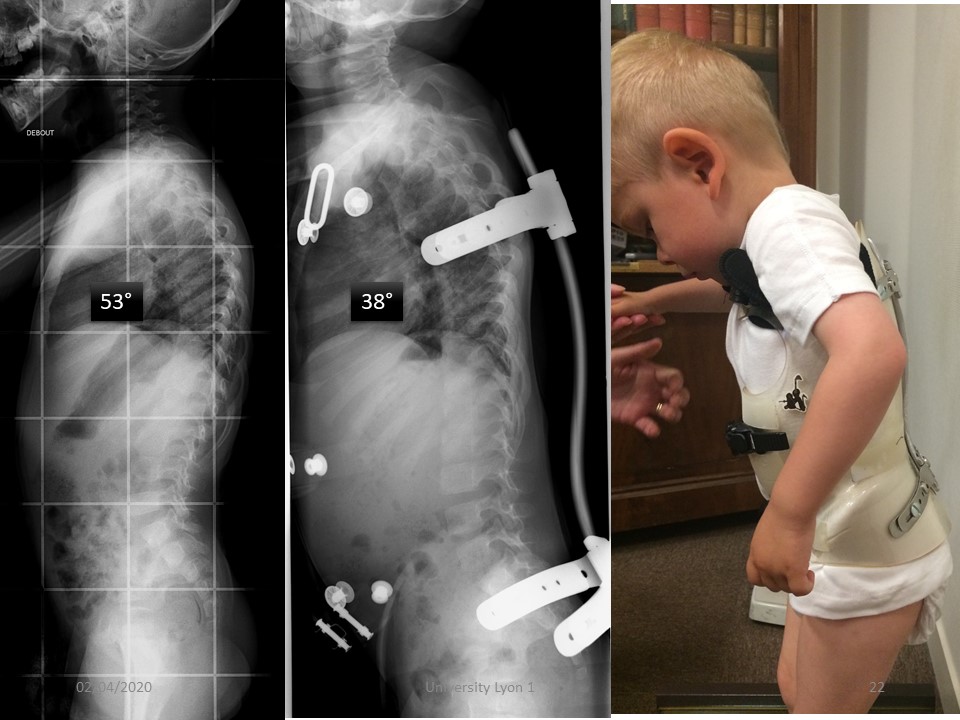 |
In the sagittal plane, the isostatic balance is correct, but the reprogramming of the extra-pyramidal sensors is incorrect when the orthosis is put in place, since the trunk is projected forward, and balance is achieved with a hip flexion.
|
 |
|
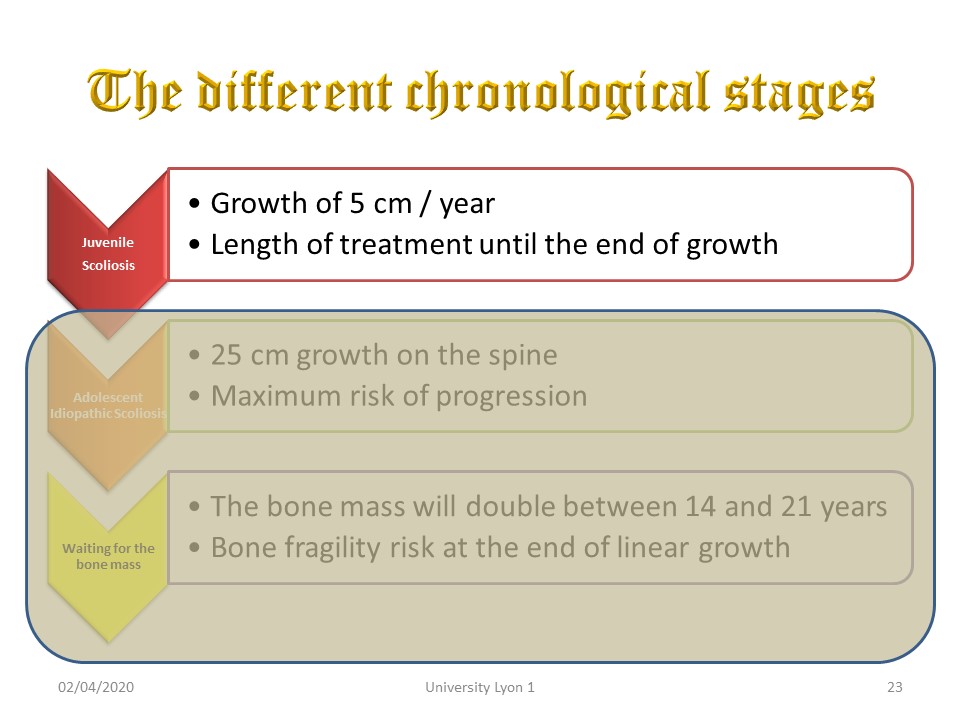 |
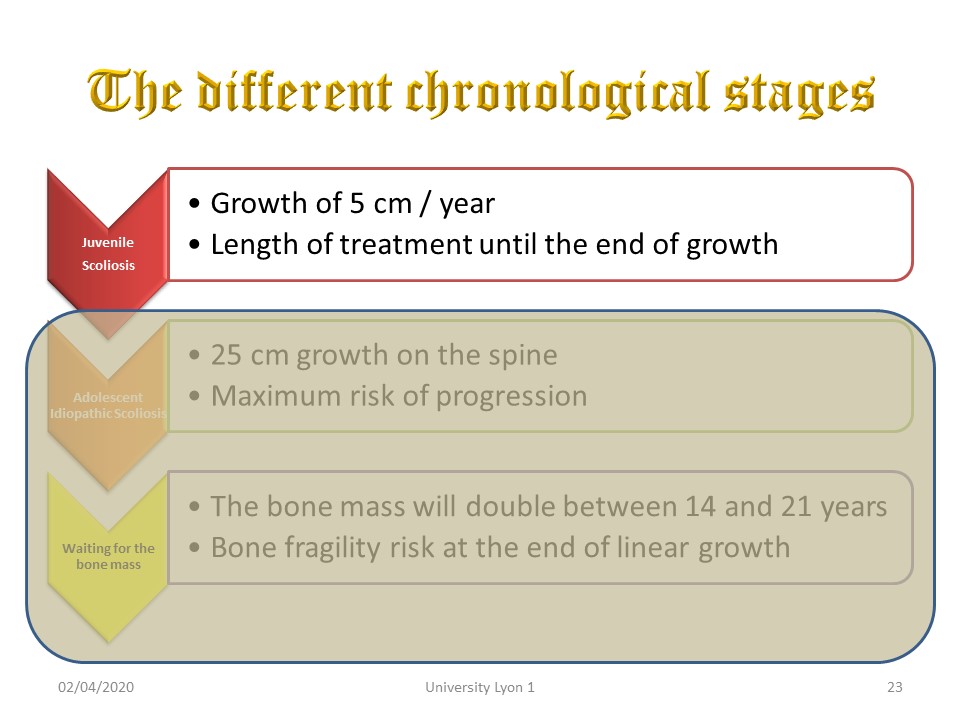
Juvenile scoliosis requires long-term treatment until the end of stature growth and is often very progressive during puberty. The child must be warned that the wearing of the brace may increase during this period.
|
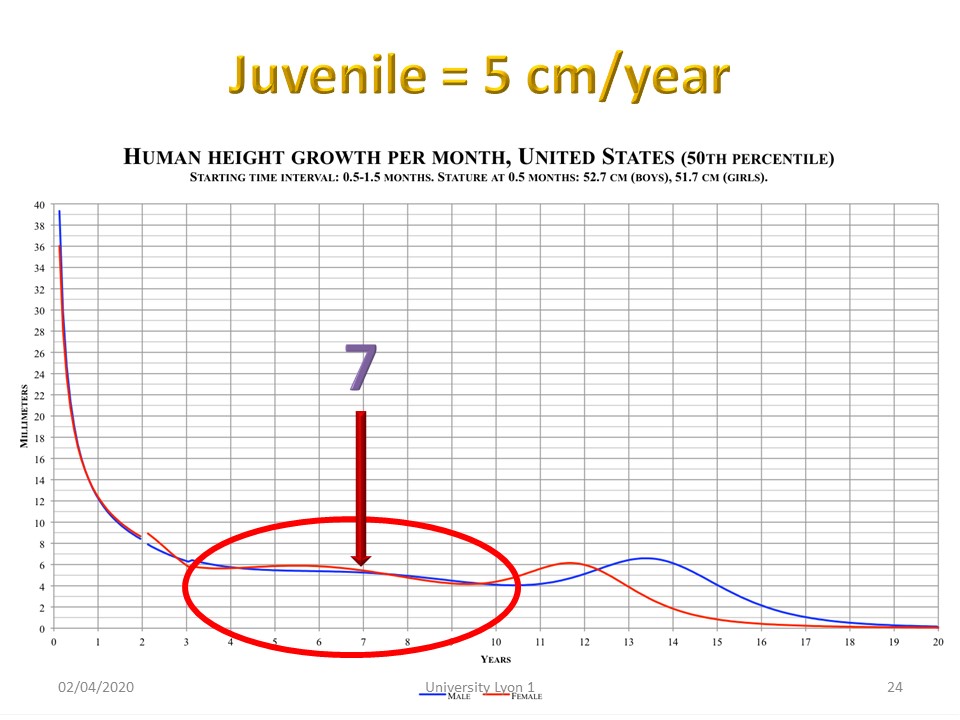 |
From 3 to 11 years in girls, the growth is 5 cm per year, about half in the lower limbs and half in the spine. Although the growth rate is the same, the age of 7 marks the beginning of adult-type locomotion.
|
 |
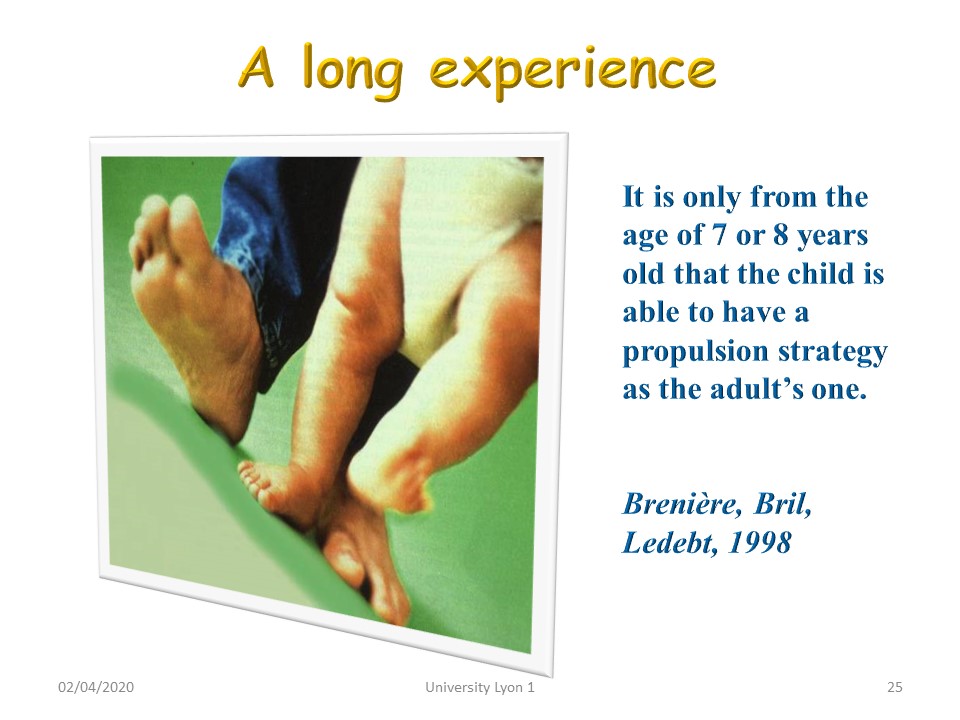
It is only from the age of 7 that the child is able to produce a walking strategy like the adult’s one. A 3 years old child runs after its centre of gravity and is unable to unroll the step. Without pelvic rotation the three-dimensionality of walking, does not exist.
|
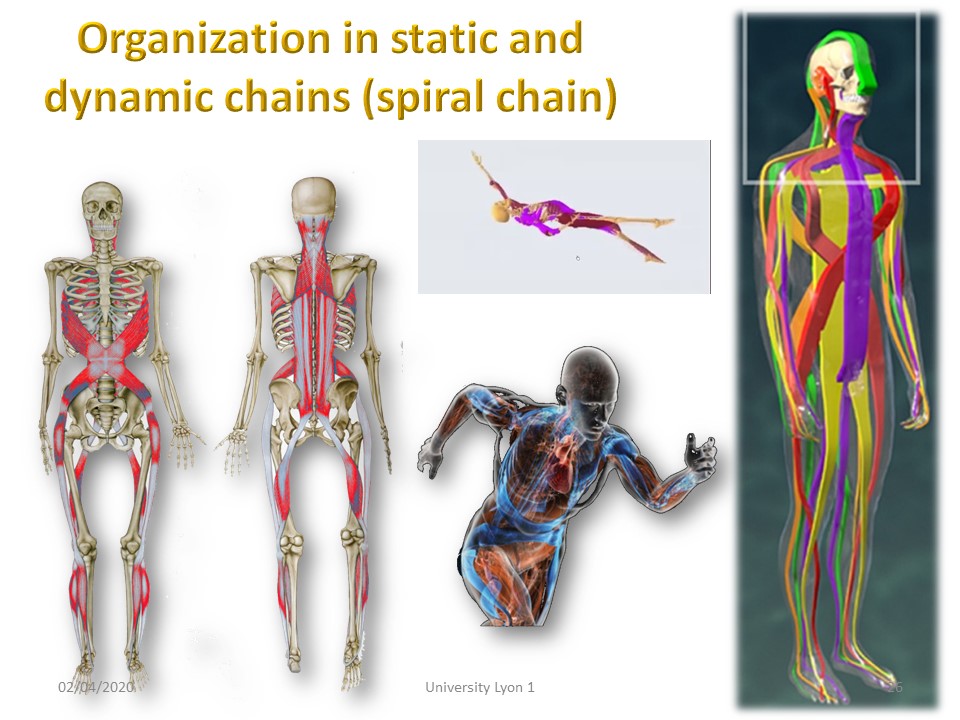 |
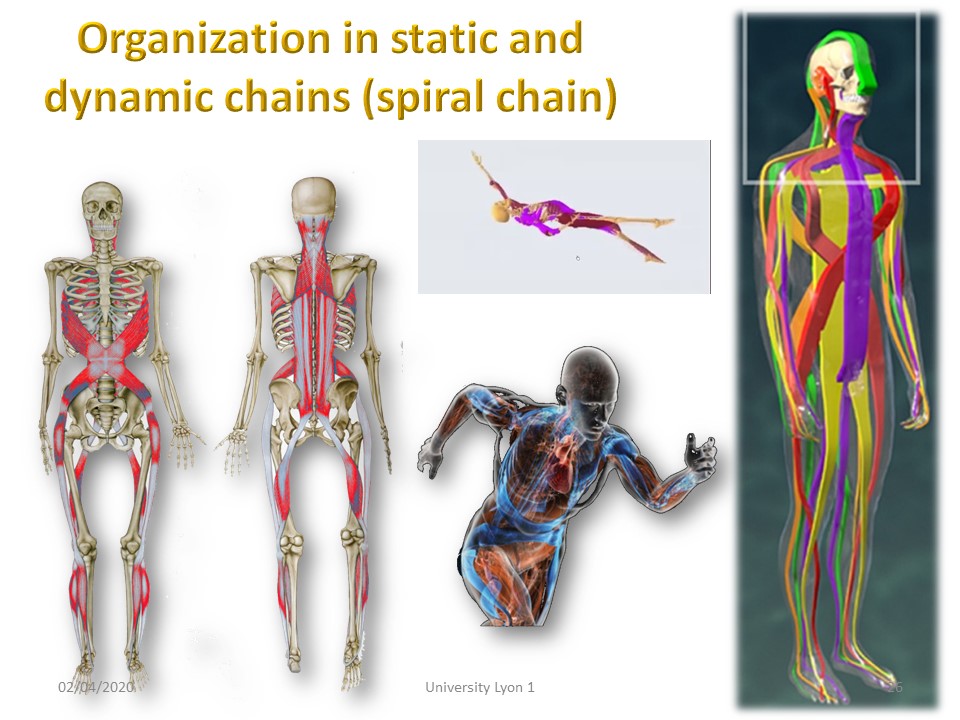
From the age of 7, the three-dimensionality is acquired, and the functional muscle chains are formed. The spiral chains are crossing each other forwards in the thoracolumbar region and backwards in the lumbosacral region.
|
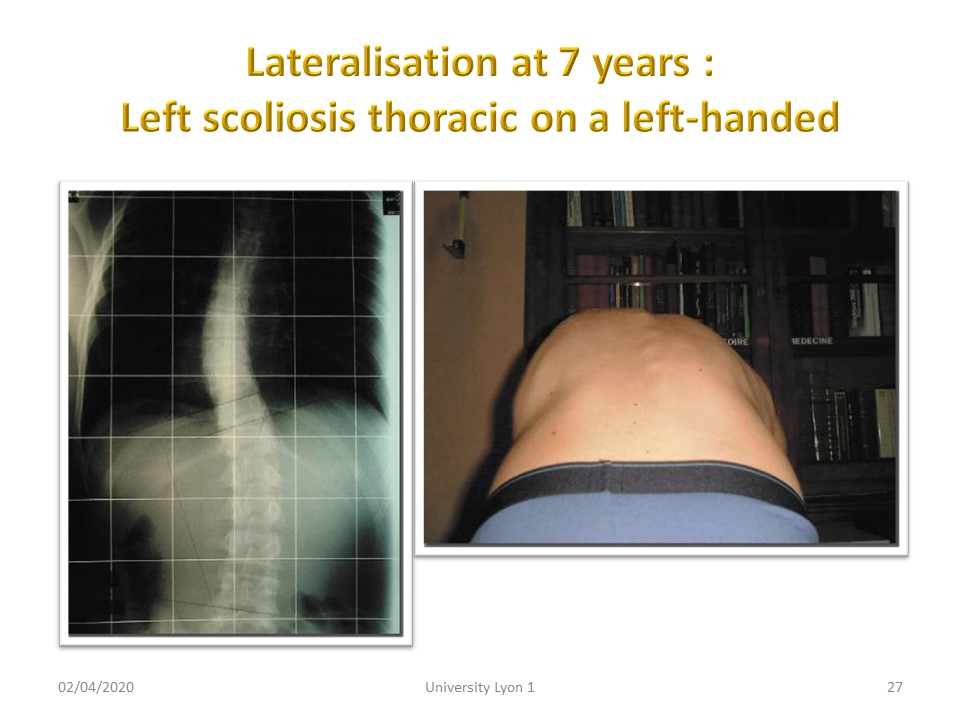 |
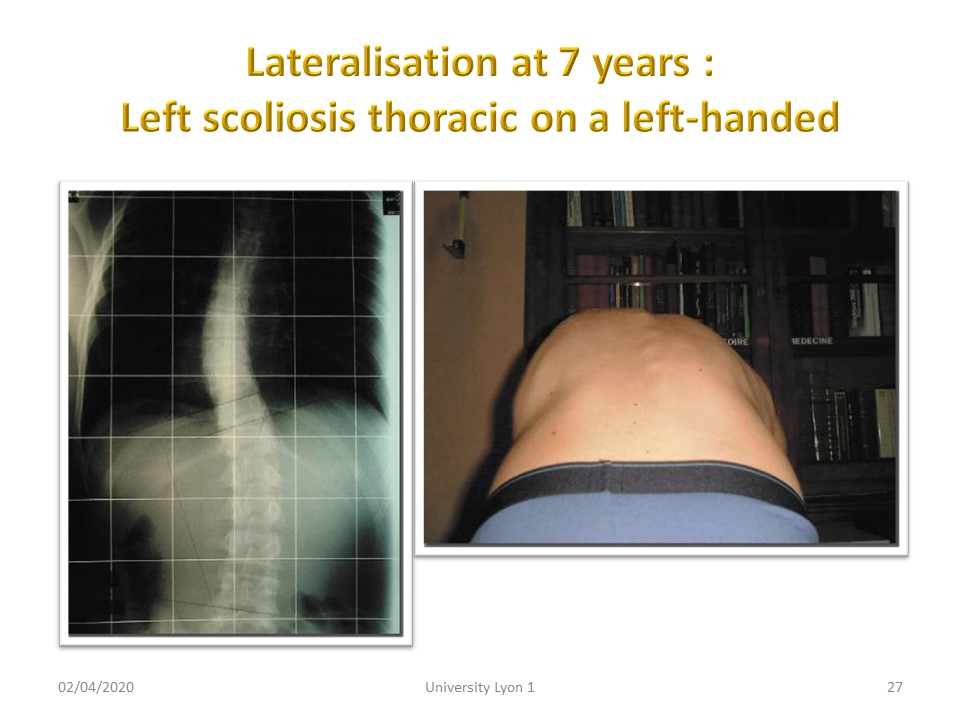
Lateralization will be completed at the age of 7. Scoliosis will be mostly right thoracic. Left handed often have left thoracic scoliosis.
|
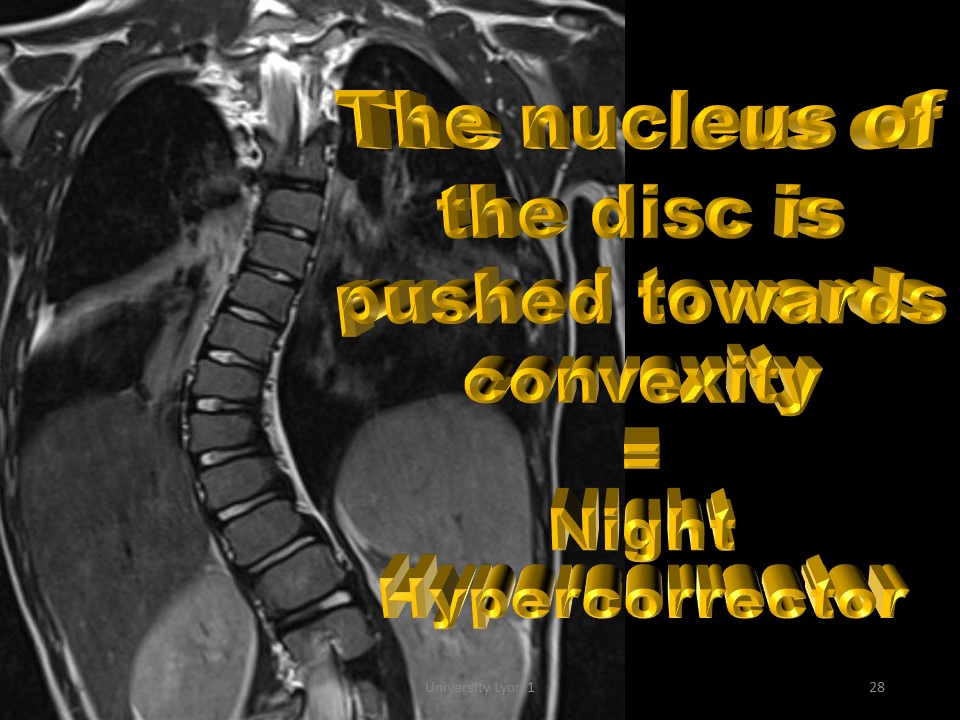 |
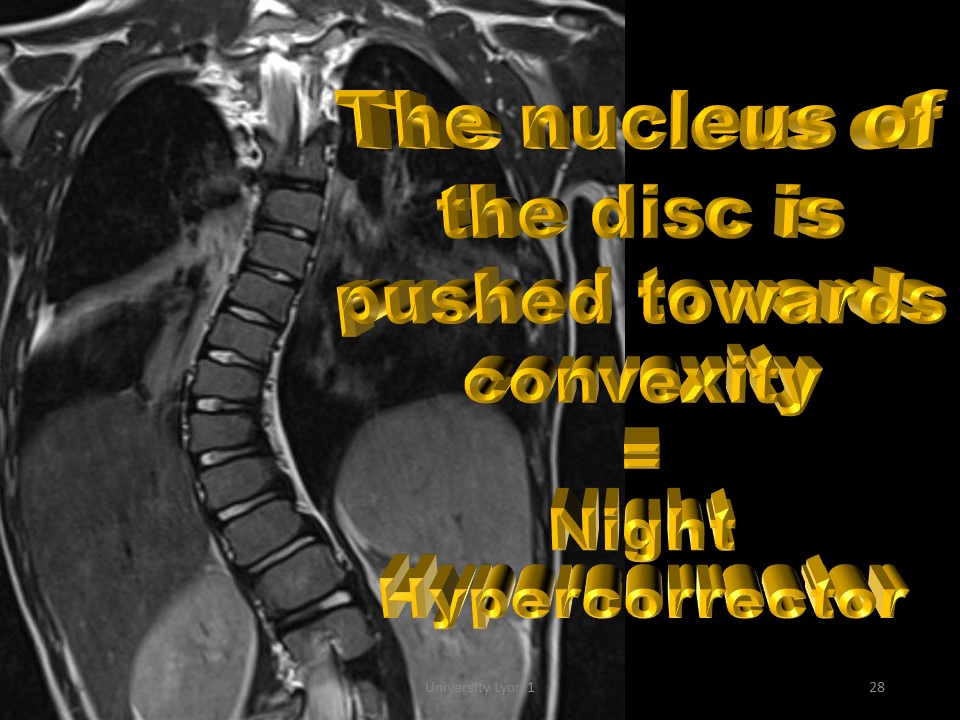
Juvenile scoliosis is flexible, and it is possible to refocus the nucleus of the apical intervertebral disc, from the convexity to the concavity by a nocturnal hypercorrective brace.
|
 |
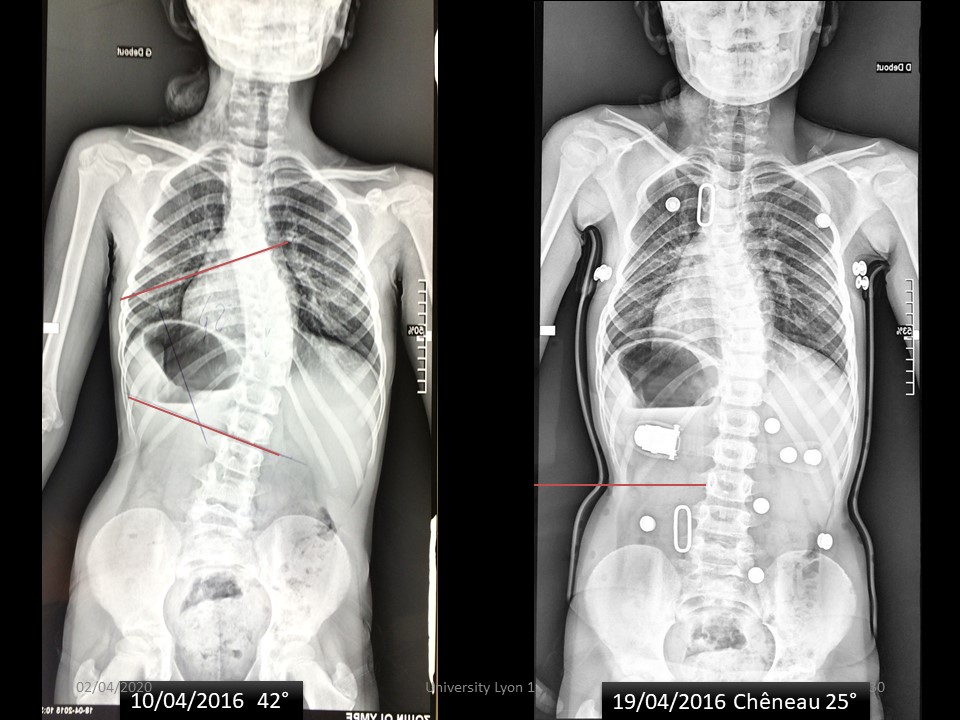
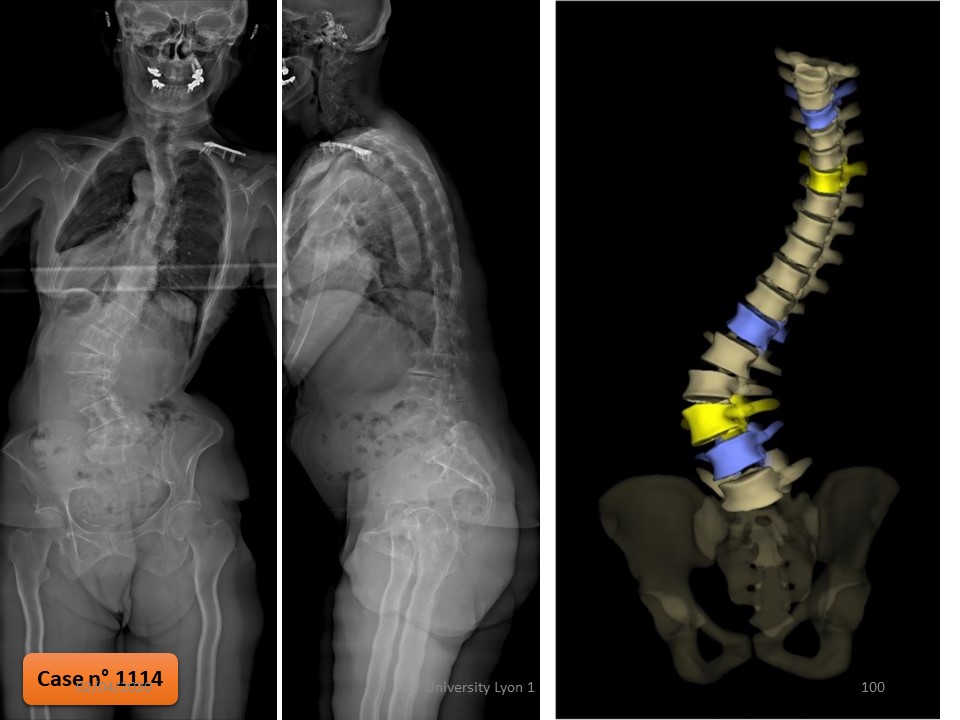
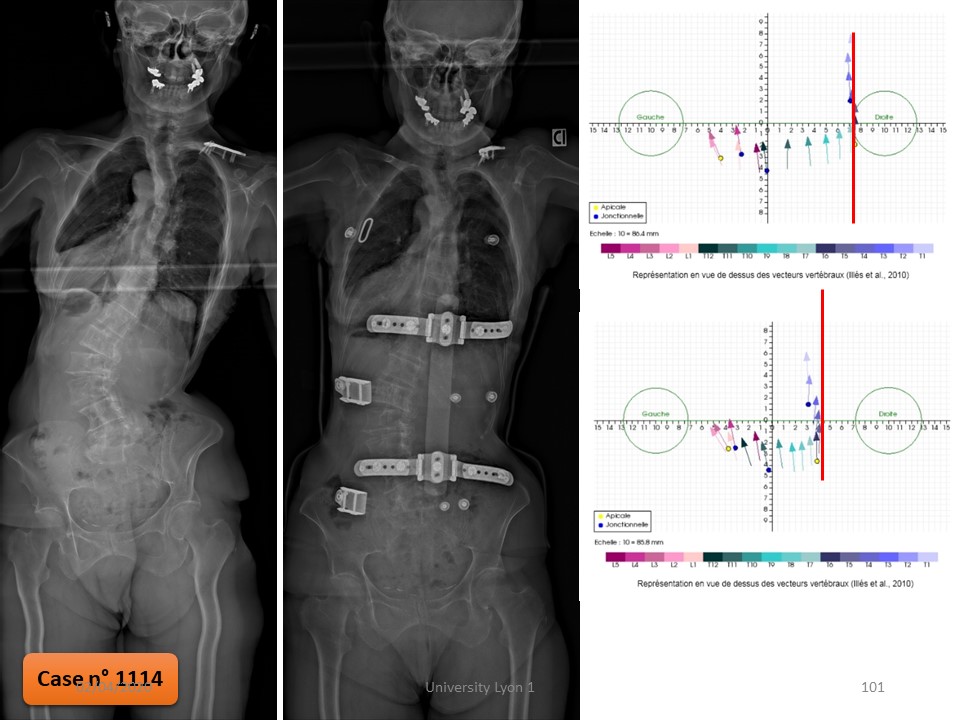
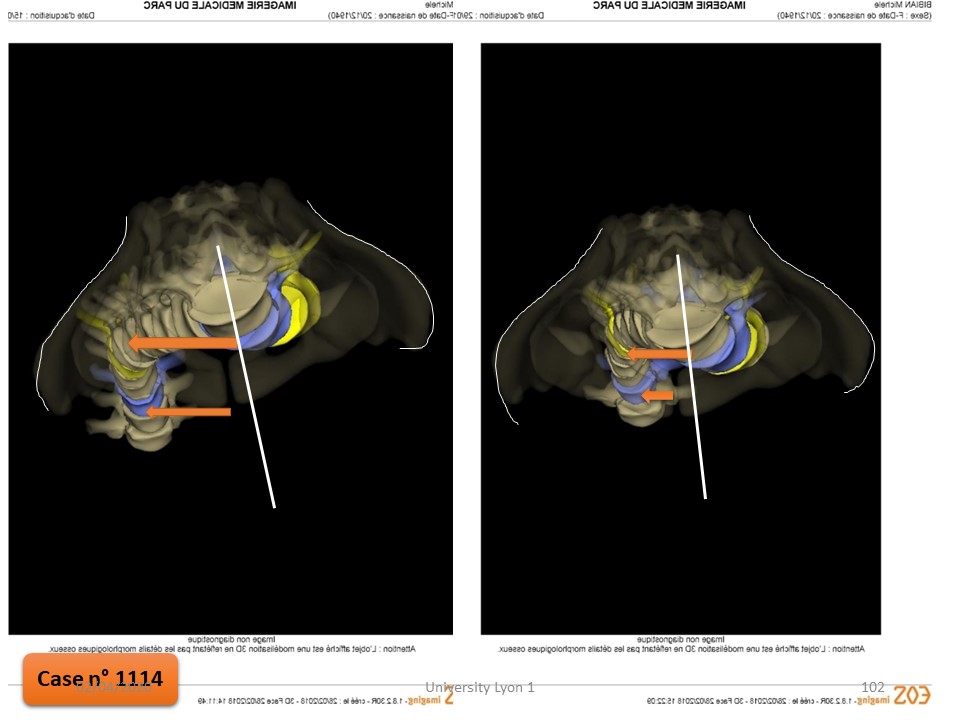
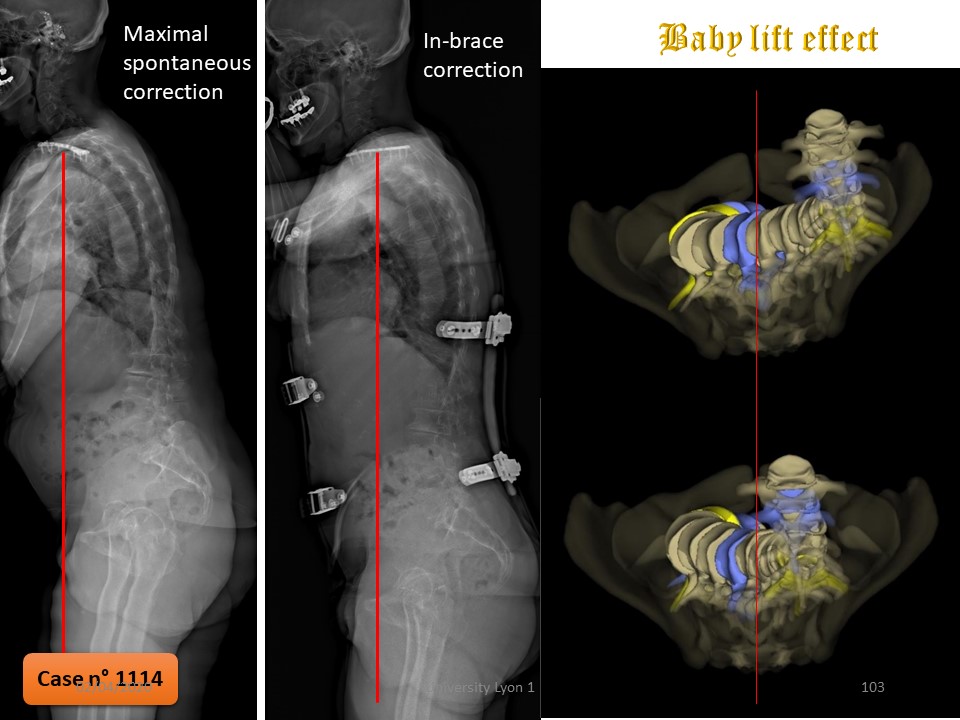
Oly scoliosis was discovered at the age of 2 years with an initial curvature of 30°. The first Milwaukee brace put in place was unsupported and a Chêneau brace by counter worn well for 3 years. Despite good compliance, the angulation progresses, and we see her at the age of 8 years with an angulation of 42°.
|
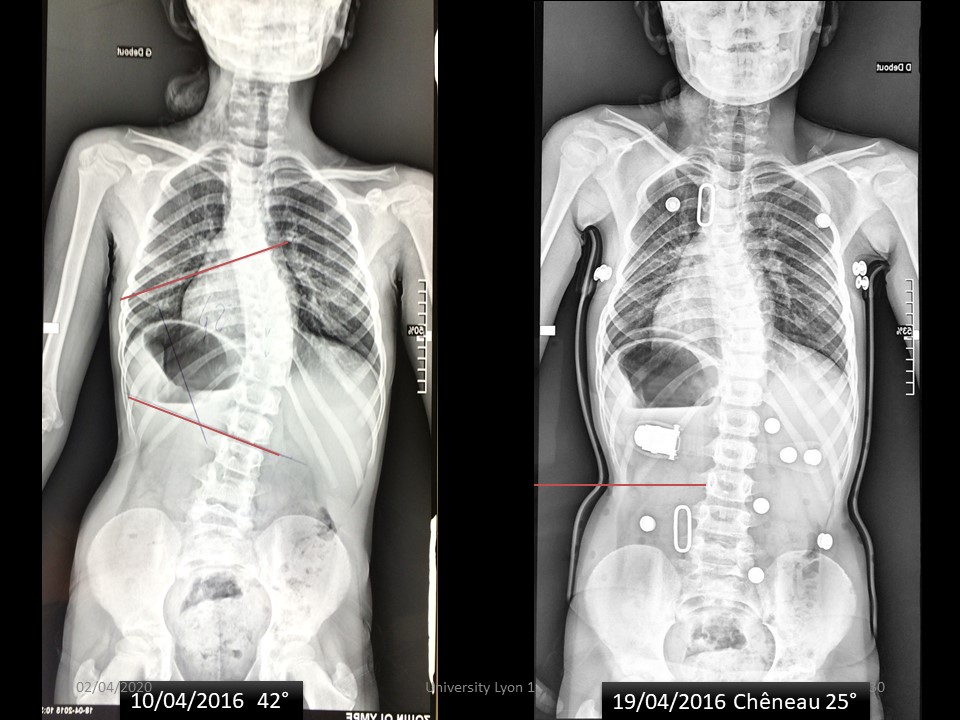 |
Under the Chêneau brace, the angulation is reduced to 25°, essentially in the lower part of the scoliosis.
|
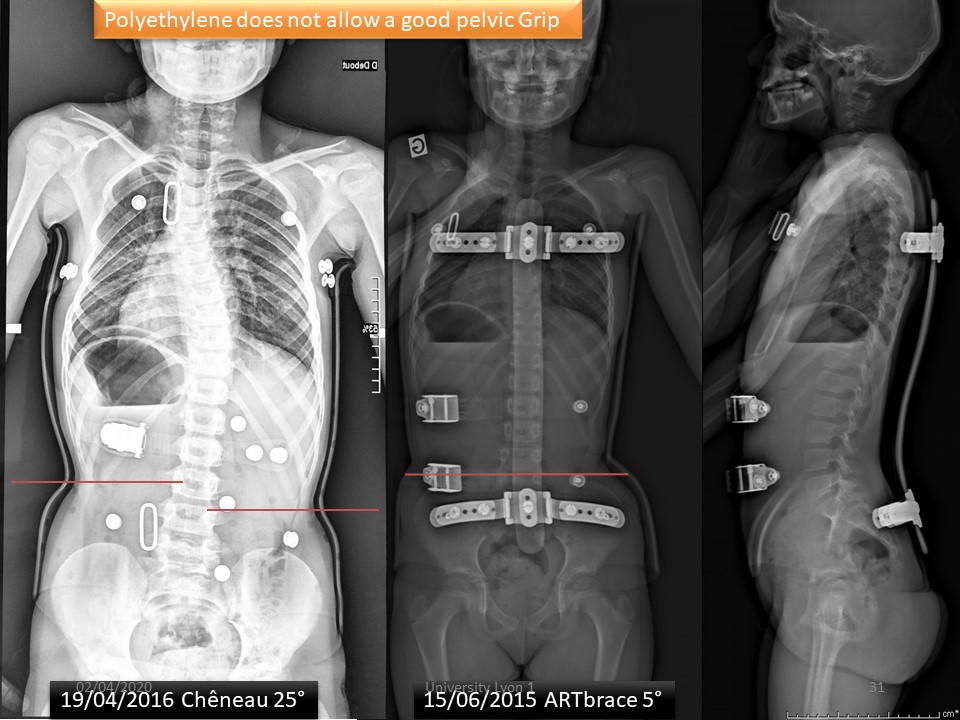 |
The ARTbrace is much more corrective in both the frontal and sagittal planes.
|
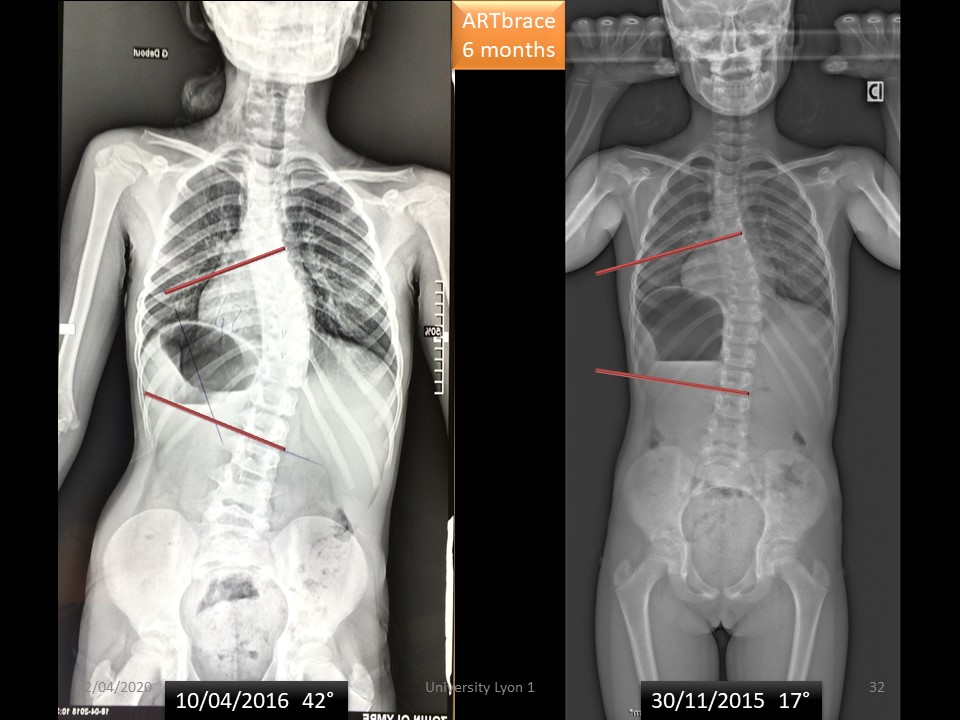 |
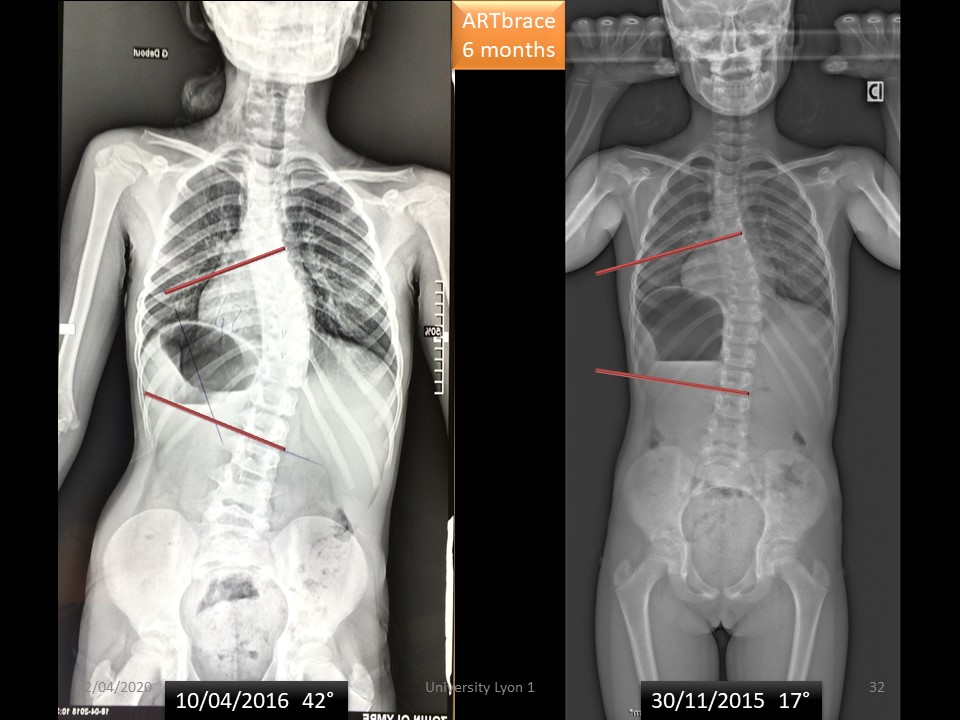
6 months after fitting, the angulation without brace is 17°.
|
 |
6 months after fitting, the angulation without brace is 17°.
|
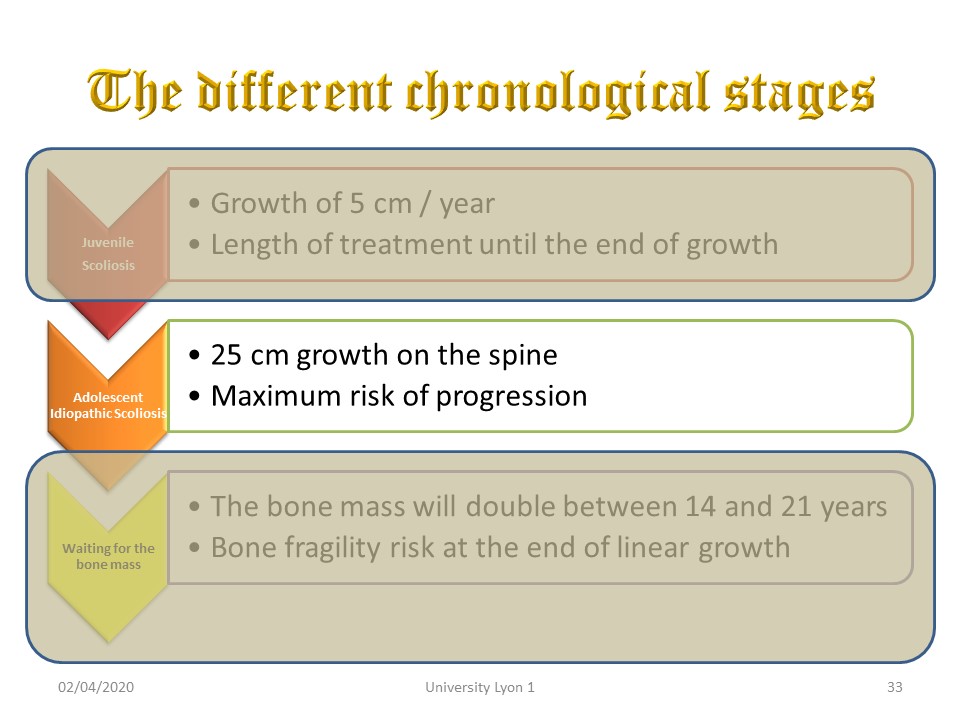 |
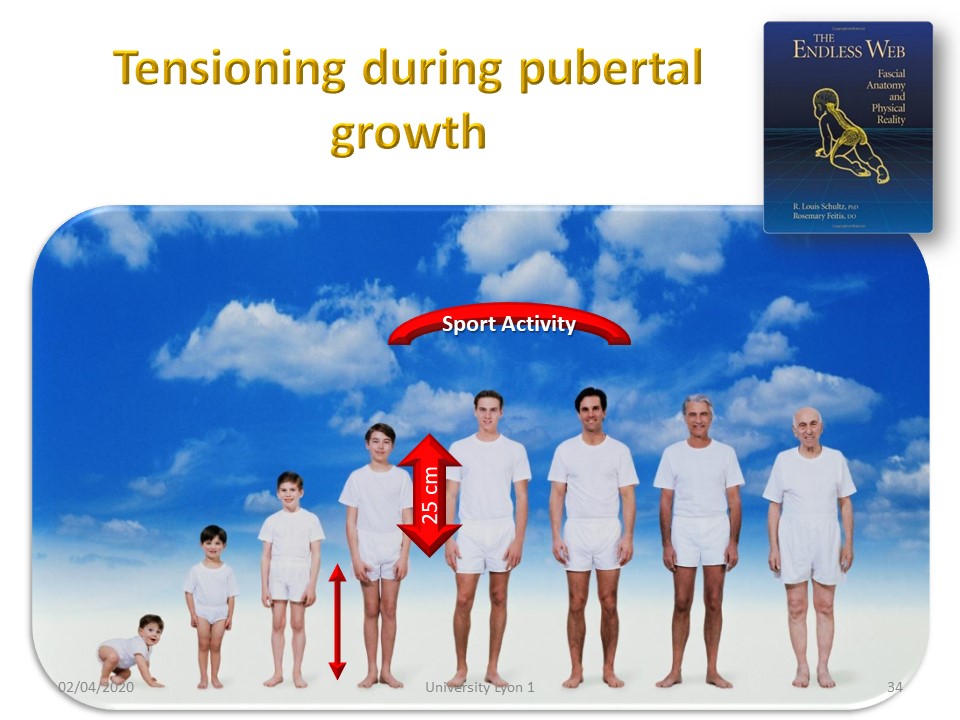
Adolescent Idiopathic Scoliosis is the usual and best-known form. The growth is 25 cm on the rachis and the risk of maximum progression. Growth occurs at the bone level and is slowed by the paravertebral Musculo-ligament chains.
|
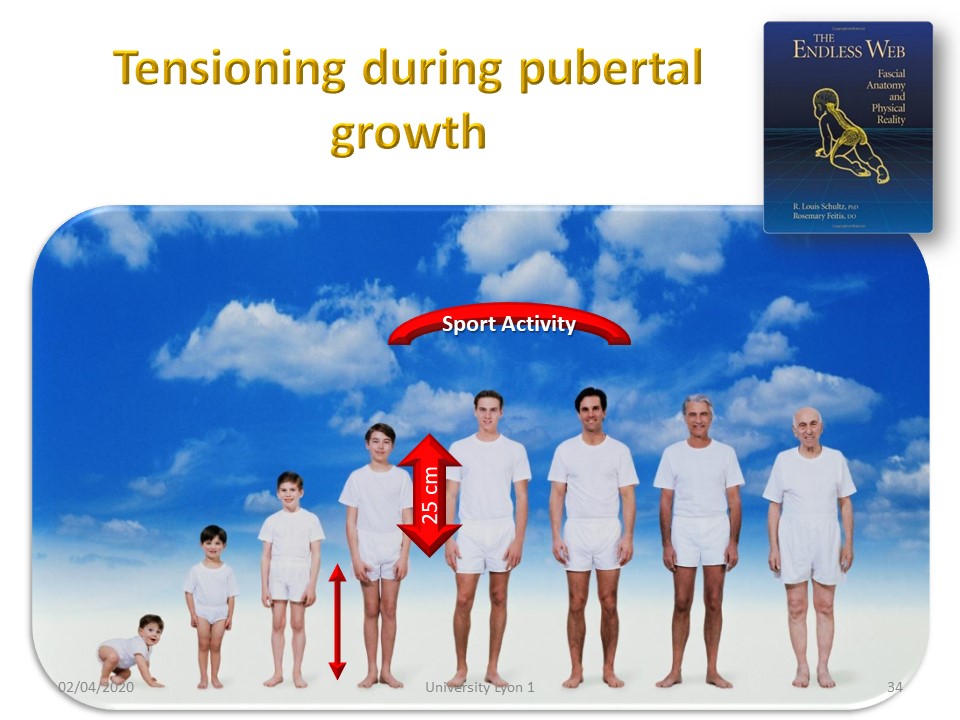 |
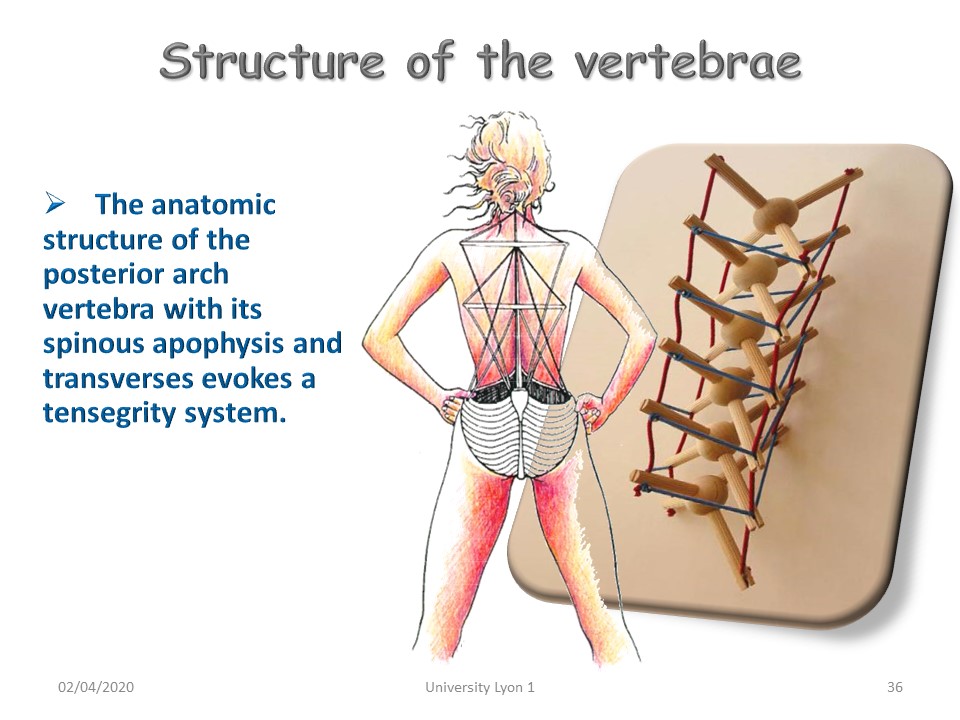
Homo sapiens is the only one to have an adolescent growth of 25 cm at the level of the spine. It is at this moment that the tensegrity is formed which will last until approximately 35 years. This is the great period of high-level sports activity. Subsequently, the intervertebral discs become compressed, the ligaments relax, and tensegrity is gradually lost.
|
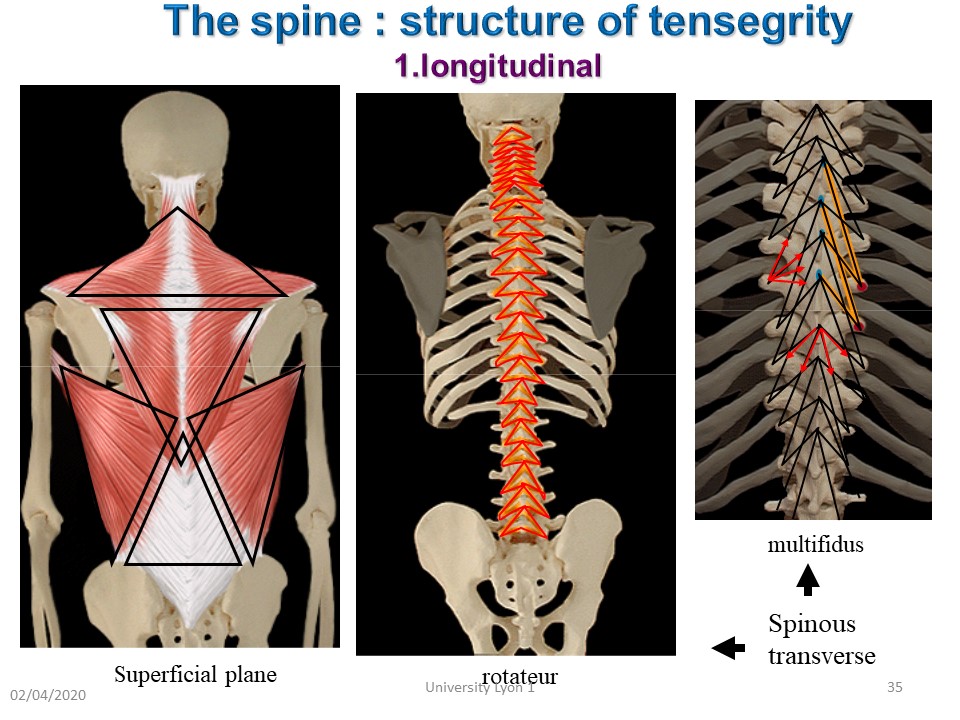 |
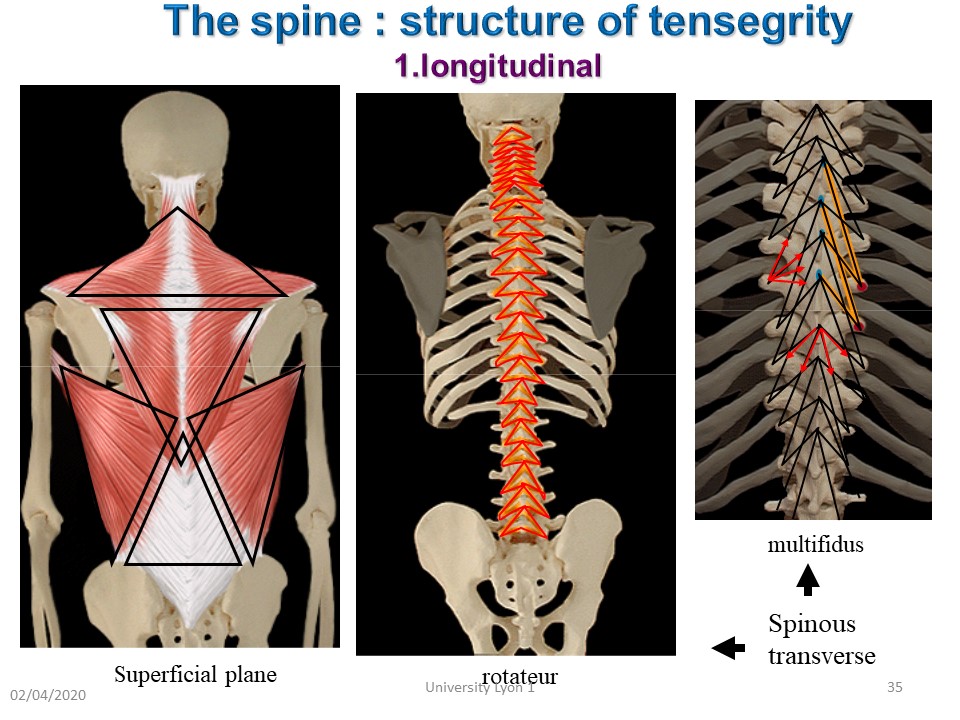
The basic structure of tensegrity is the triangle which offers a best stability, but the muscle structure paravertebral as deep as superficial has a triangular structure. The intervertebral disc is also a tensegrity structure.
|
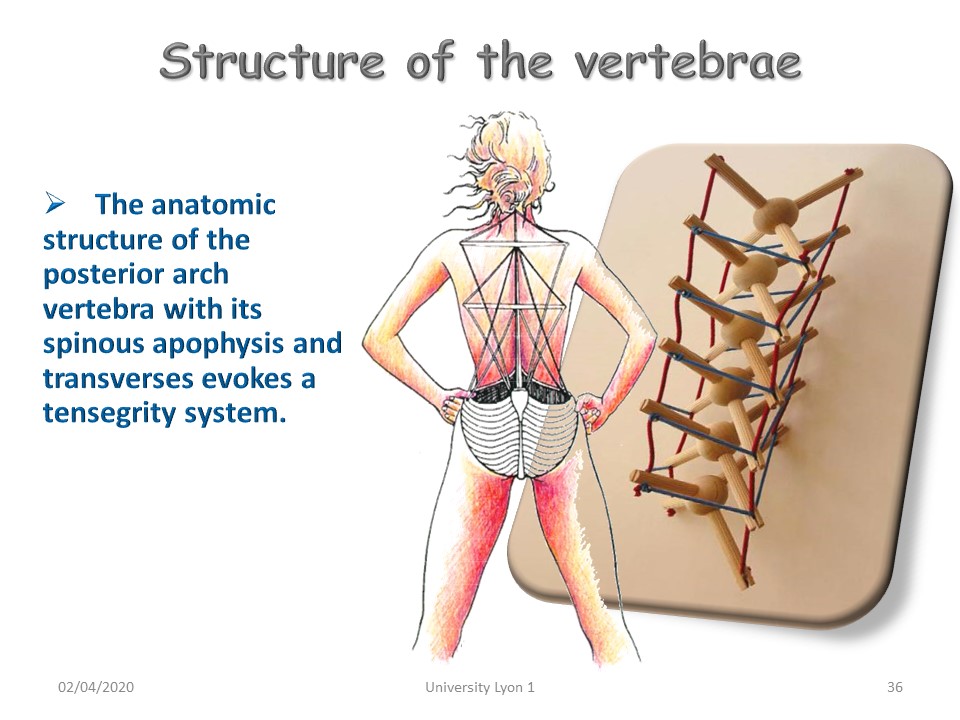 |
The anatomic structure of the posterior arch of the vertebra with its spinous apophysis and transverses oriented in triangle, evokes a tensegrity system. Tensegrity requires mobility of all segments. With scoliosis the apical area is stiff, while the end vertebrae are more mobile.
|
 |
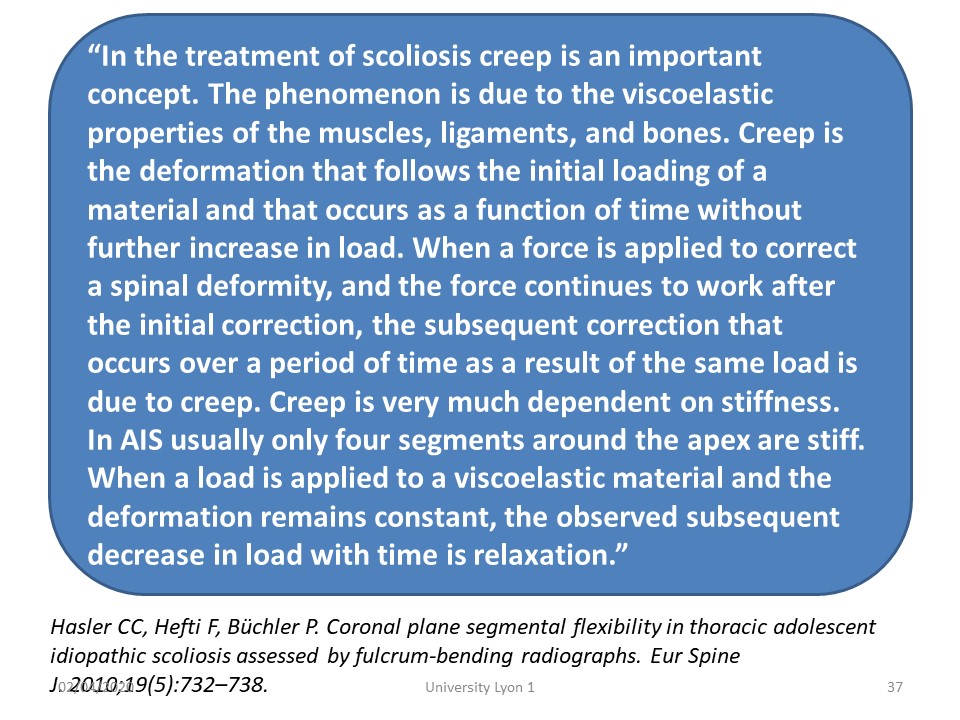
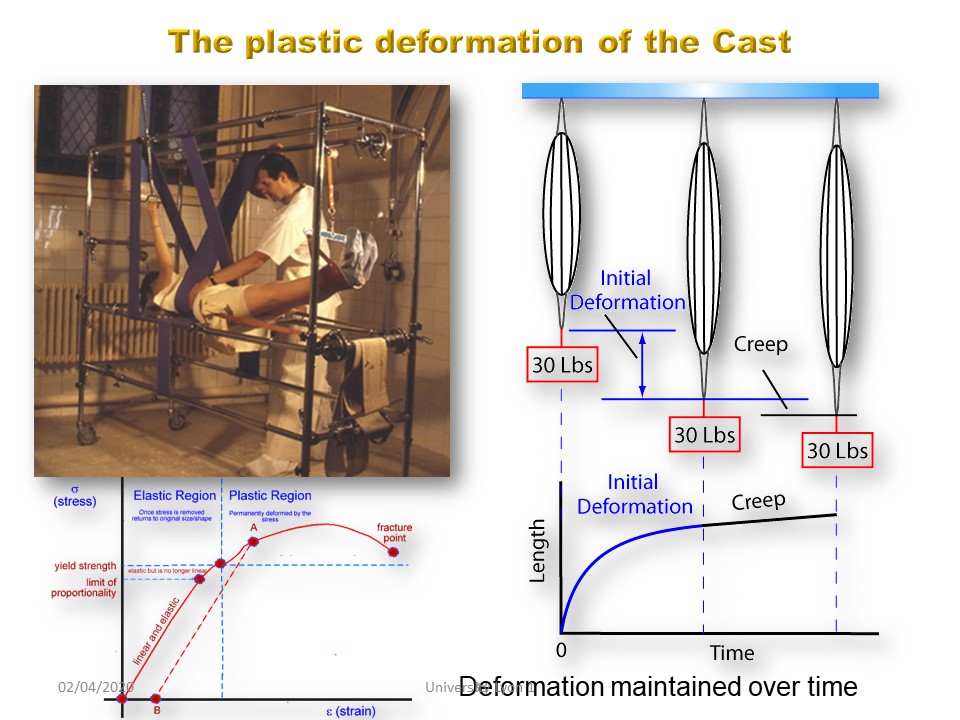
Only the plastic deformation obtained by the plaster cast or a hypercorrective brace, worn in "total time", can restore a favourable tensegrity. “In the treatment of scoliosis creep is an important concept. The phenomenon is due to the viscoelastic properties of the muscles, ligaments, and bones. Creep is the deformation that follows the initial loading of a material and that occurs as a function of time without further increase in load. When a force is applied to correct a spinal deformity, and the force continues to work after the initial correction, the subsequent correction that occurs over a period of time as a result of the same load is due to creep. Creep is very much dependent on stiffness. In AIS usually only four segments around the apex are stiff. When a load is applied to a viscoelastic material and the deformation remains constant, the observed subsequent decrease in load with time is relaxation.”
|
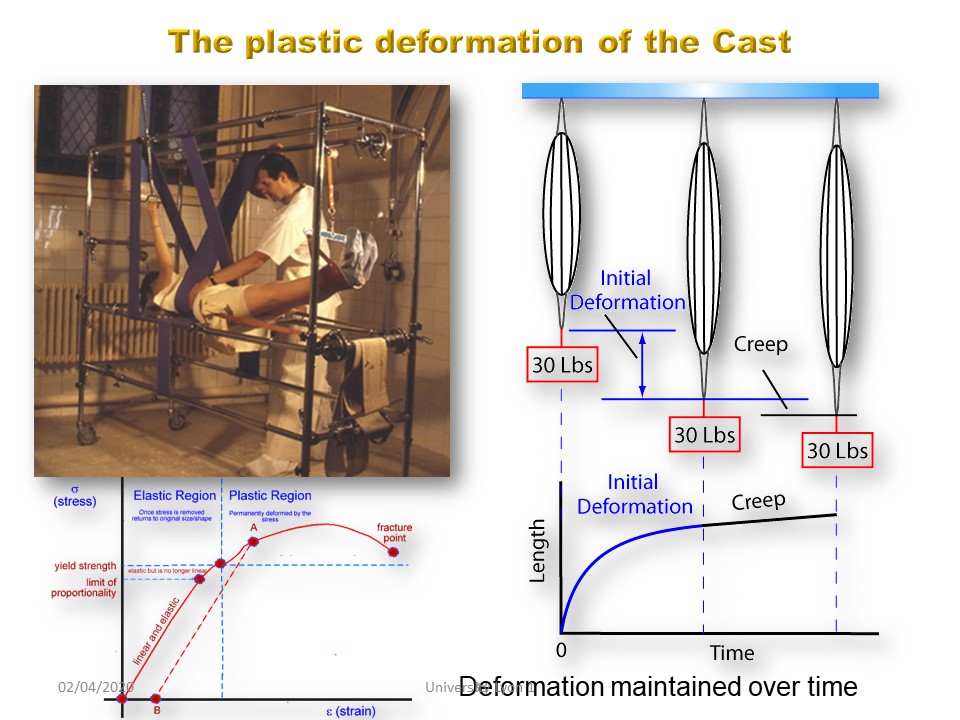 |
To restore Tensegrity in spine deviations, the length of the ligaments must be changed. This is why the characteristic of Lyon conservative treatment is the creep, that is to say the plastic deformation or change of length of the viscoelastic paravertebral structures (geometric non-linearity). The creep requires a continuous tension of 1 to 4 months, this mean a “total time” of cast or brace.
|
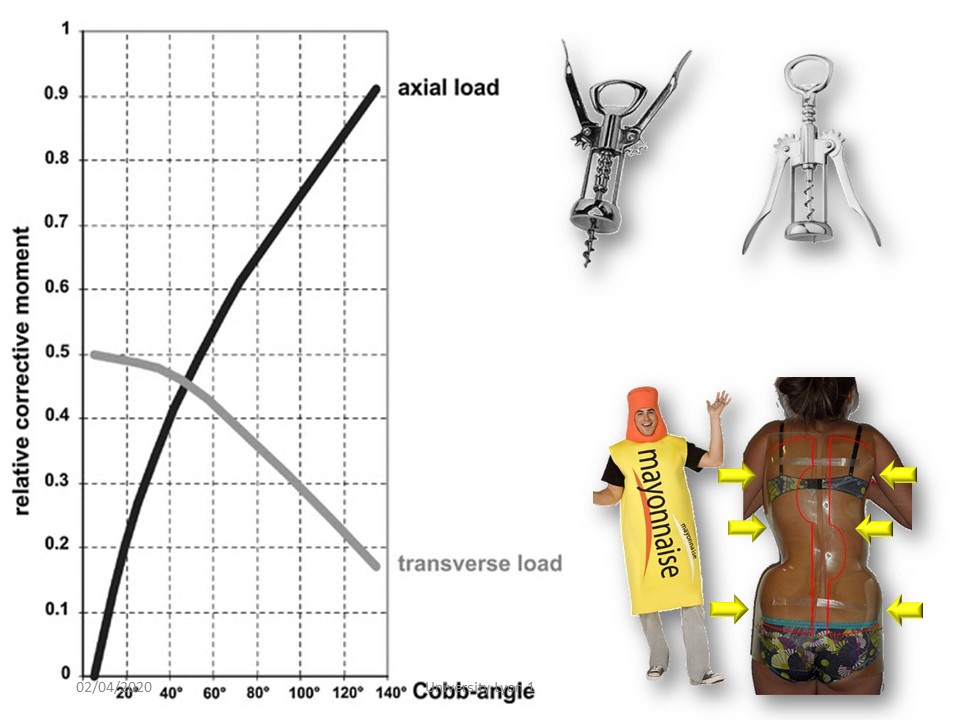 |
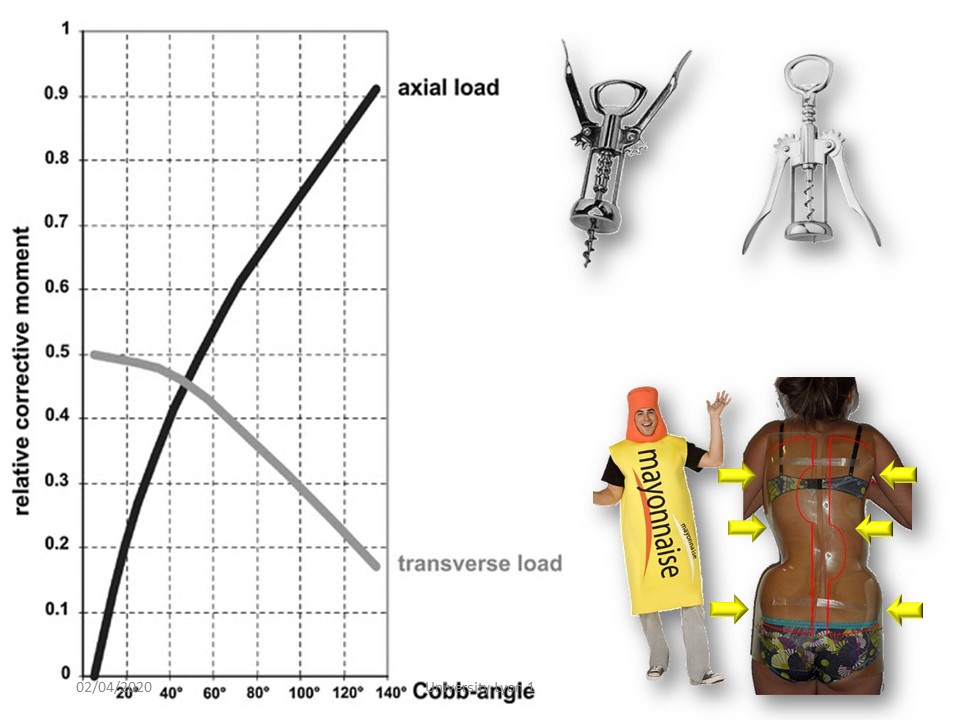
In adolescence, the corrective forces associate translation along the vertical axis (lever corkscrew effect) and rotation in a horizontal plane. For a small angulation, the rotation in the transversal plane is more important. Over 40°, the translation along the vertical axis becomes the predominant component.
|
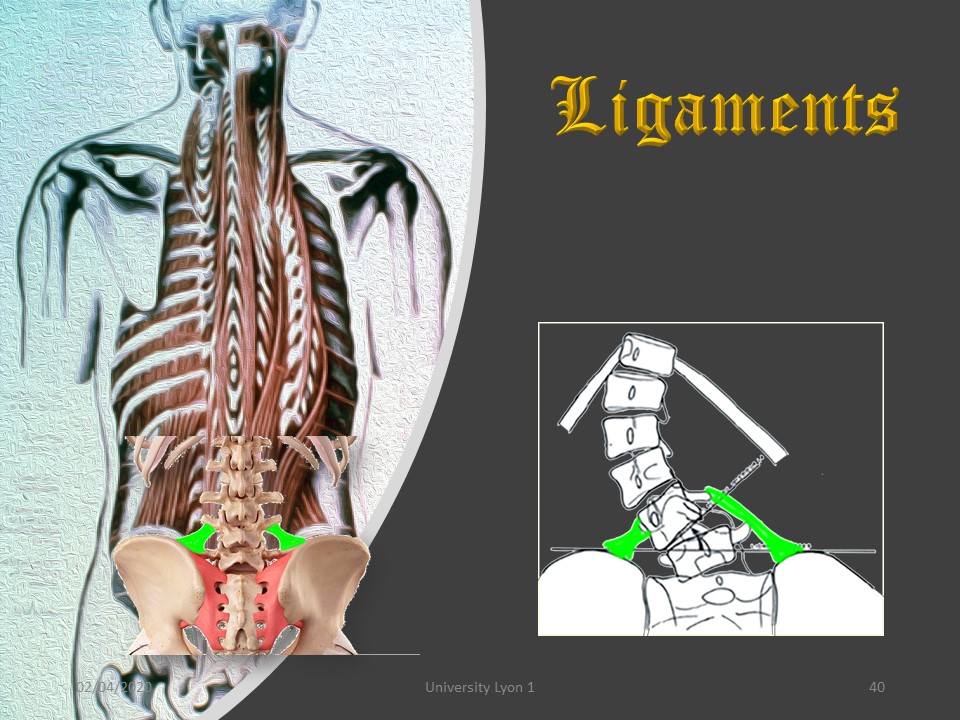 |
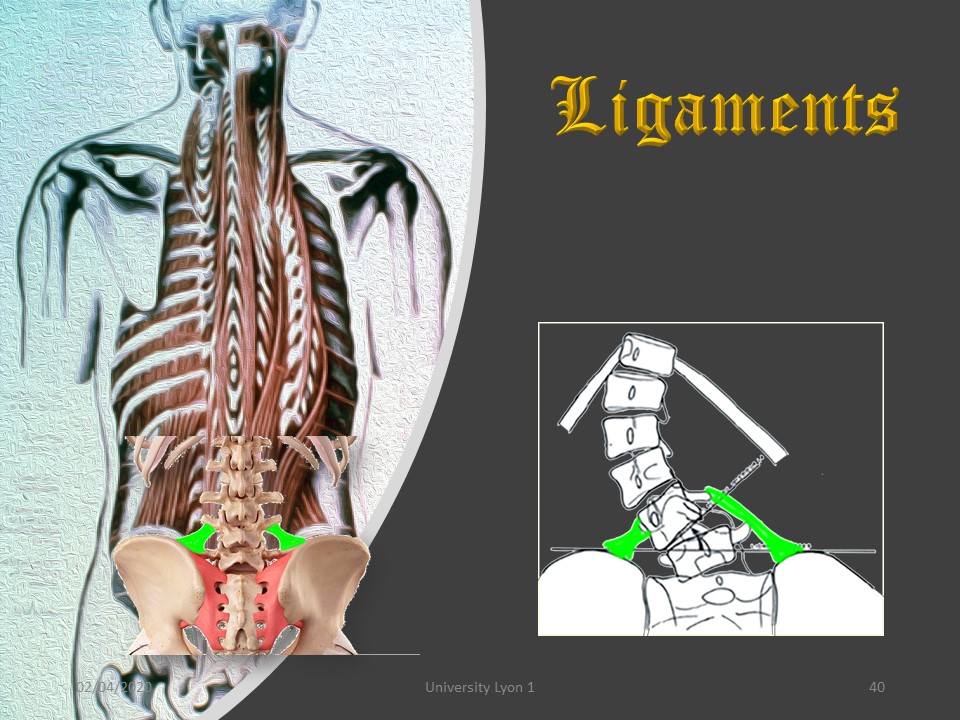
From the Rhesus monkey the ilio-lumbar muscles have been transformed into ligaments which are sometimes asymmetrical with tilt of L4 and increase of the iliolumbar angle. The problem is that stretching the short convex ilio-lumbar ligament, accentuates lumbar scoliosis.
|
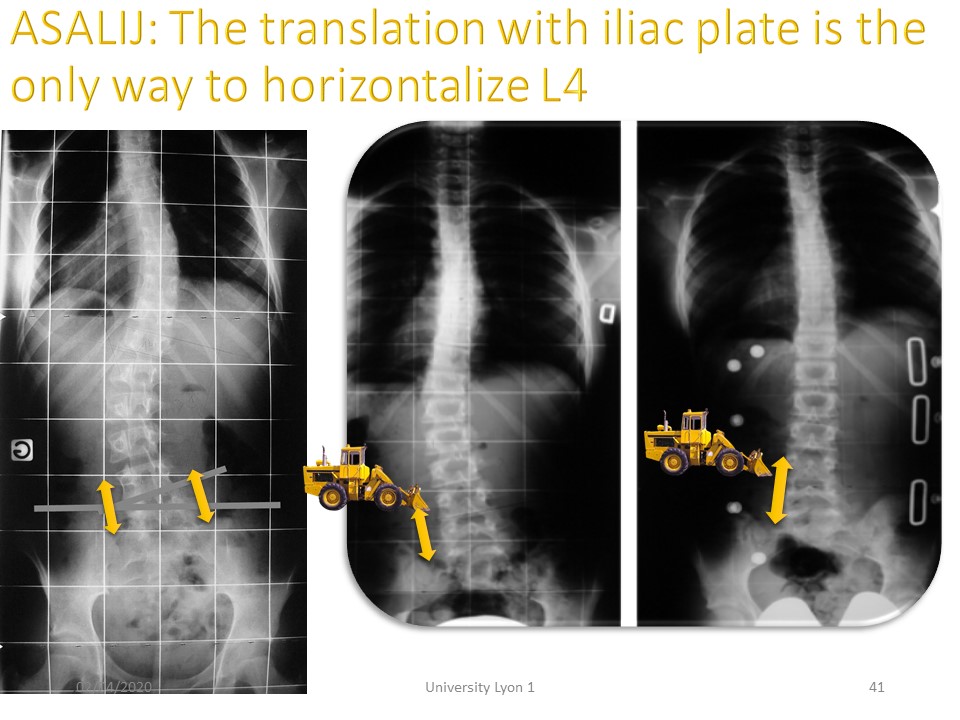 |
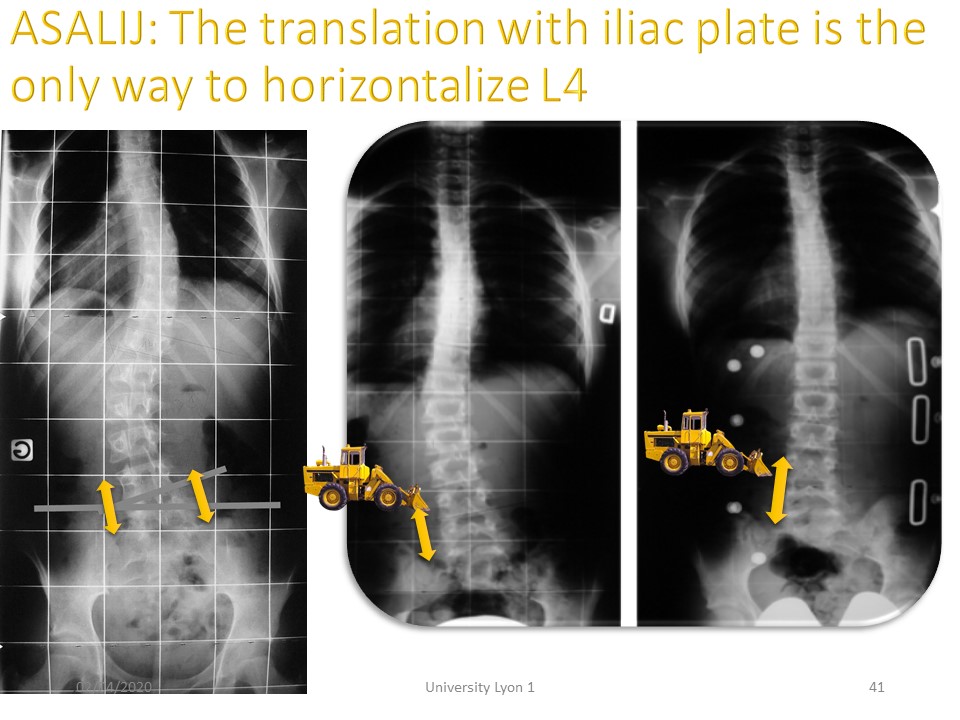
Radiology confirms that the only way to stretch the ilio-lumbar ligament is to translate this lumbar spine to the concavity. This is usually enough to straighten the entire lumbar spine.
|
|
Comment in the certification part of the website
To view the full video presentation register for the certification course” www.scoliosisandspineonlinelearning.com
|
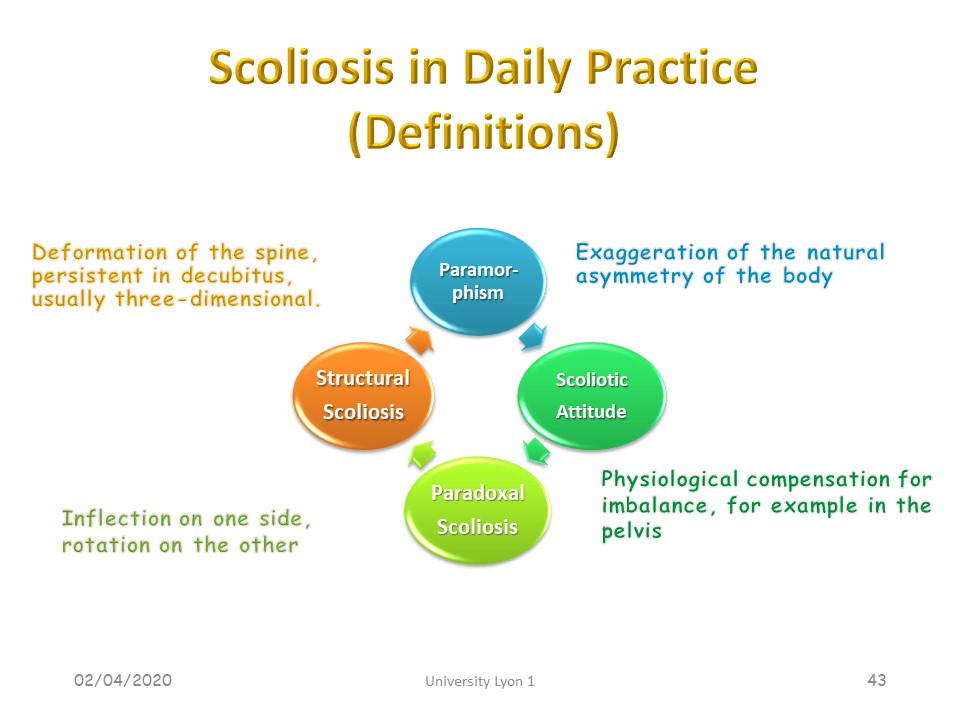 |
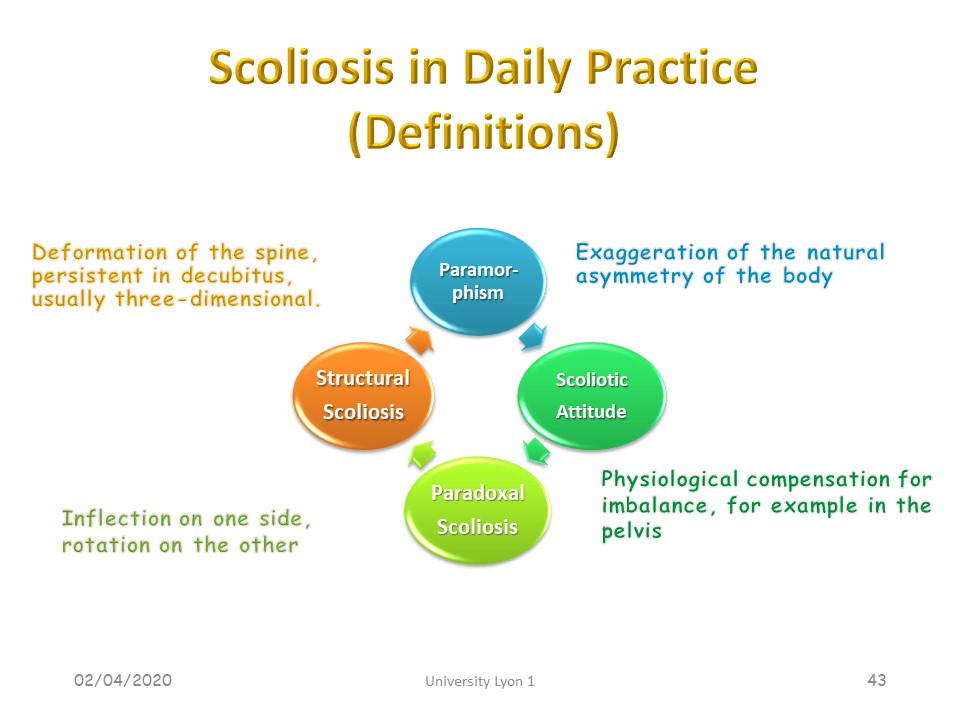
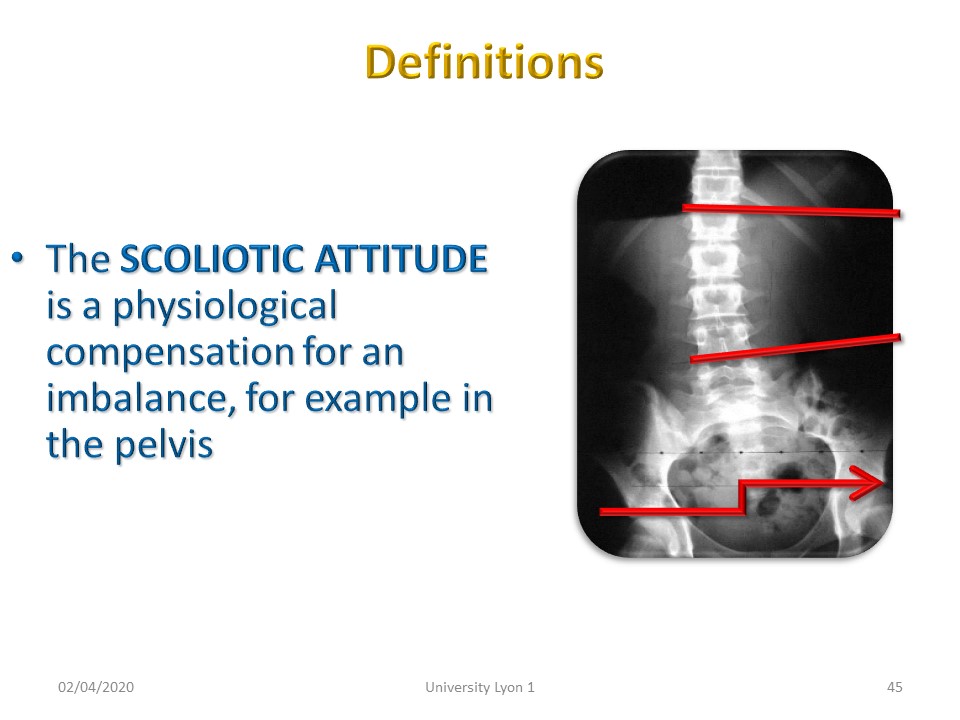
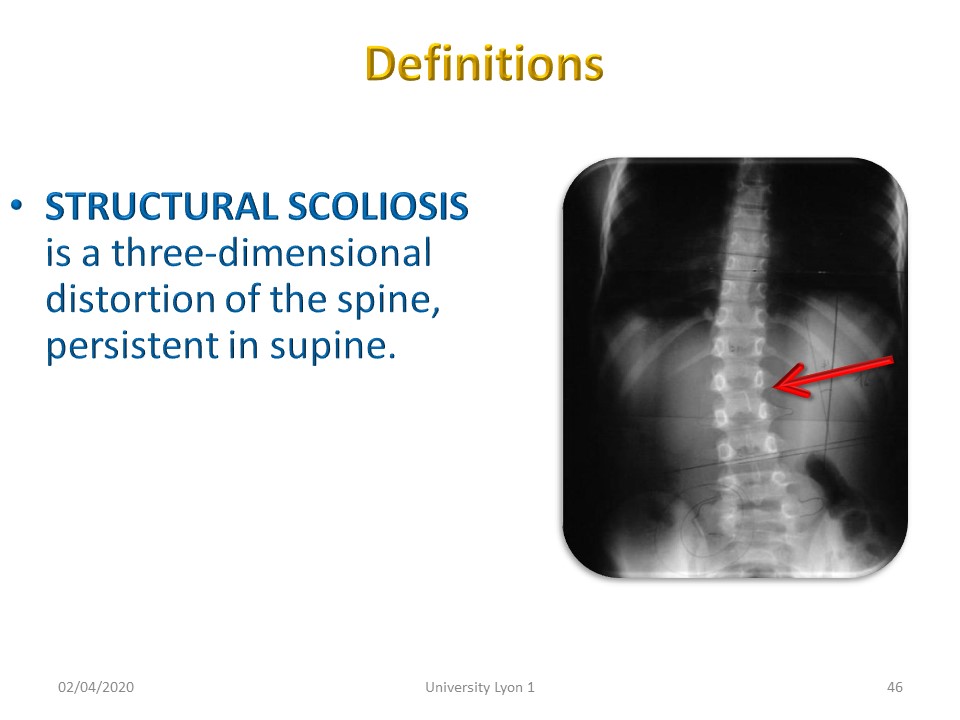
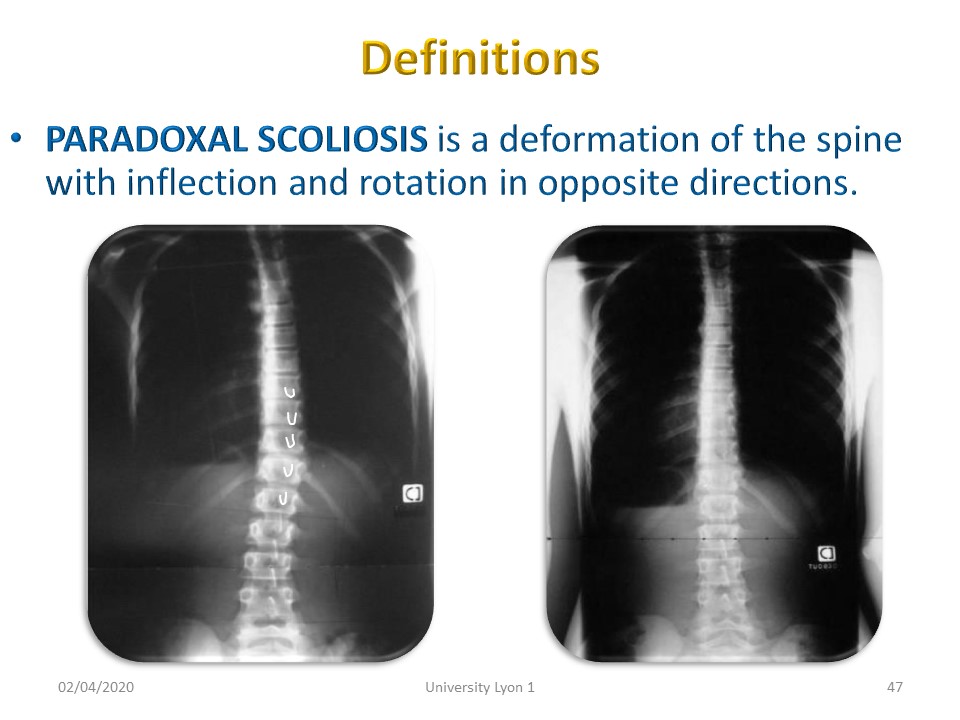
For small curvatures between 0 ° and 20 °, it is necessary to specify the difference between paramorphism or functional scoliosis, scoliotic attitude, paradoxical scoliosis and structural scoliosis.
|
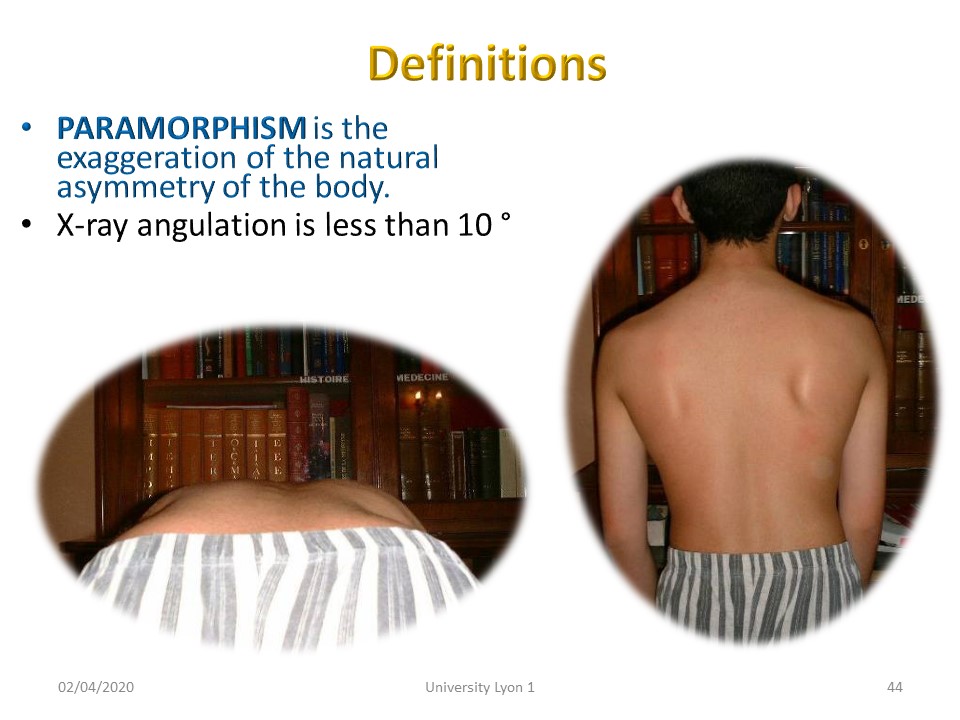 |
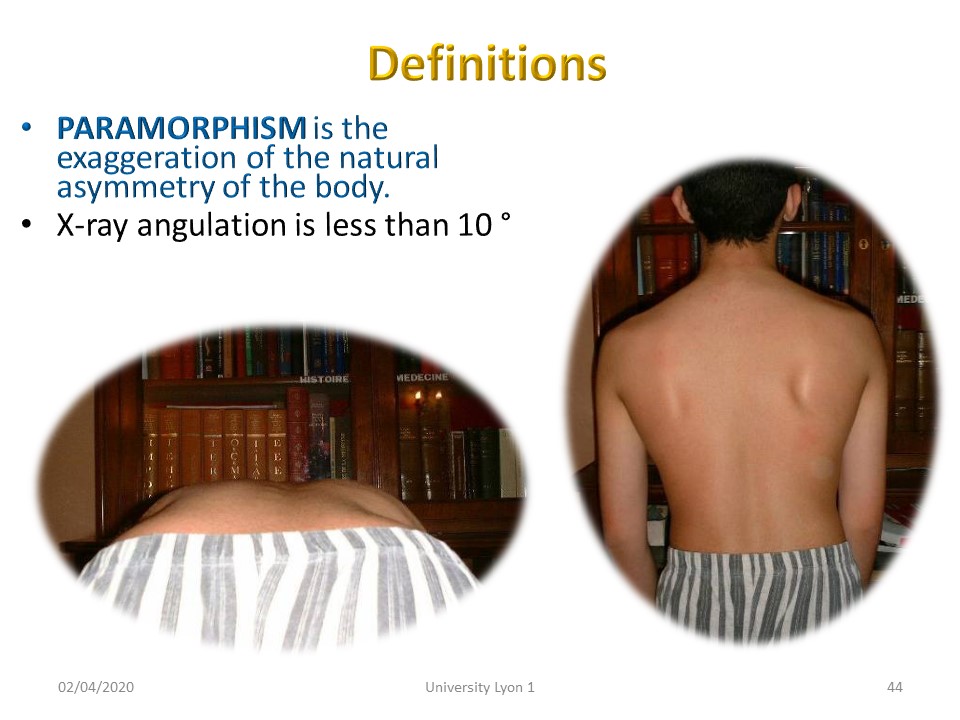
Paramorphism is the exaggeration of the natural asymmetry of the trunk and is often noted in children intensely practicing a sport. The angulation of scoliosis is less than 10 ° and the rib hump of a few mm. Paramorphism does not require specific physiotherapy. The parents are told the Adam’s test.
|
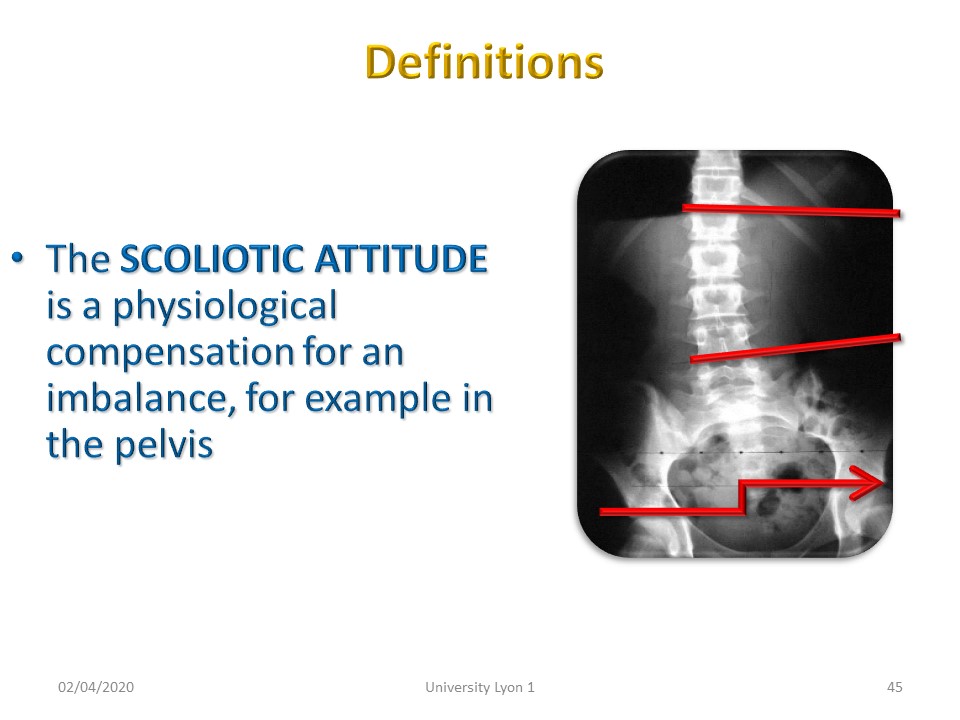 |
The SCOLIOTIC ATTITUDE is a physiological compensation for an imbalance, for example in the pelvis. It allows the head to rebalance on the line of gravity. The rotation is minimal. There is however a risk of decompensation in structural scoliosis and the problem of compensation by shoe lift, which we will study more in detail.
|
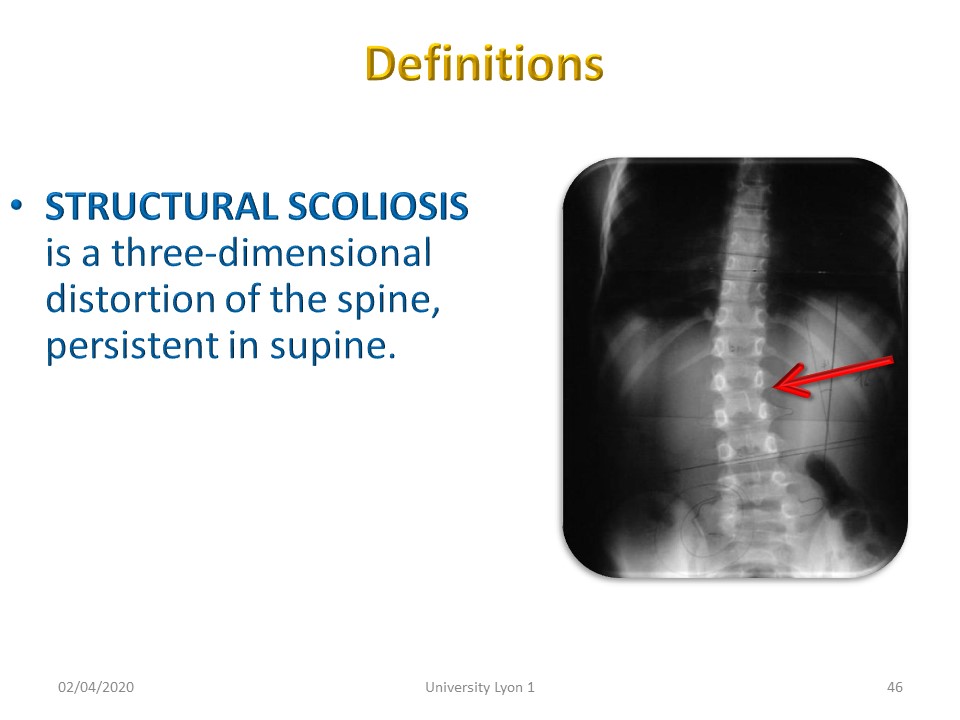 |
Structural scoliosis is a three-dimensional deformity of the spine, not reducible. Asymmetry affects bone, growth cartilage, intervertebral disc, paravertebral Musculo-ligamentous structures. There is a delay in the maturation of the posture and balance systems. Beyond 20 °, the linear evolution has been described by Duval-Beaupère according to the vicious circle of Ian Stokes.
|
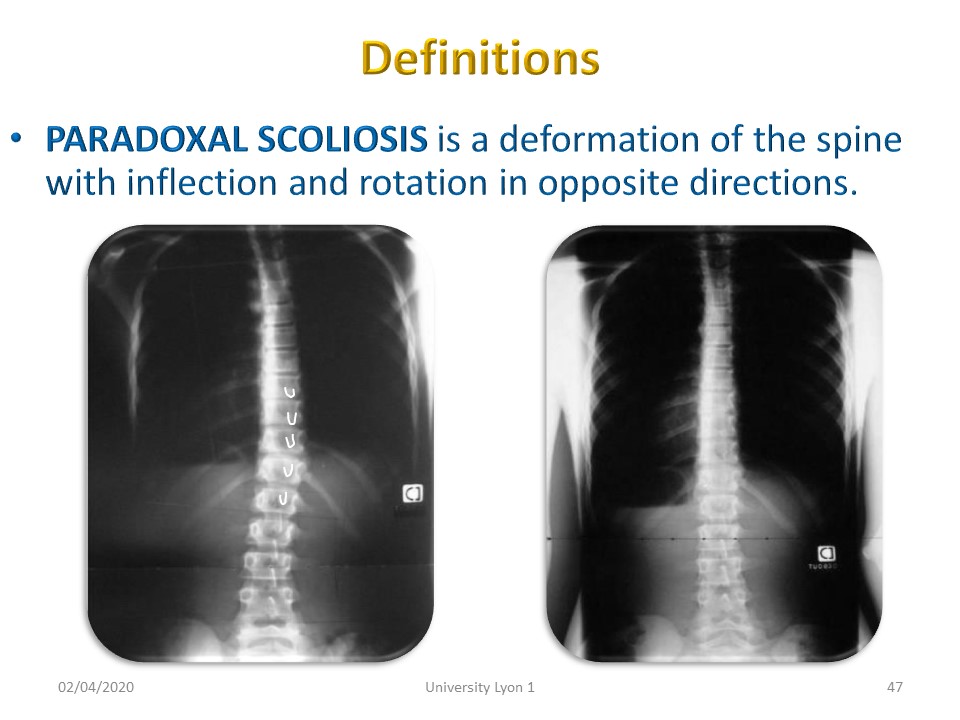 |
Paradoxal scoliosis is a particular form of scoliosis with a rightward inflection, but rotation of the vertebral body to the left. The vertebral body turns to the left and the spinous process is projected towards the right convexity. This is one of the rare cases where the evolutionary prognosis is favourable.
|
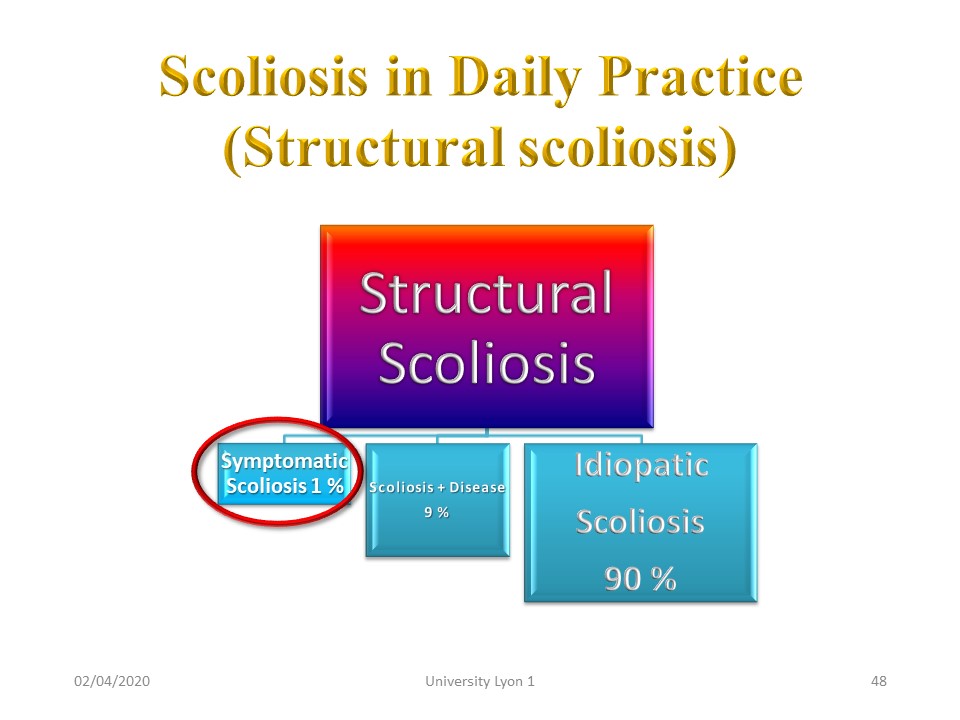 |
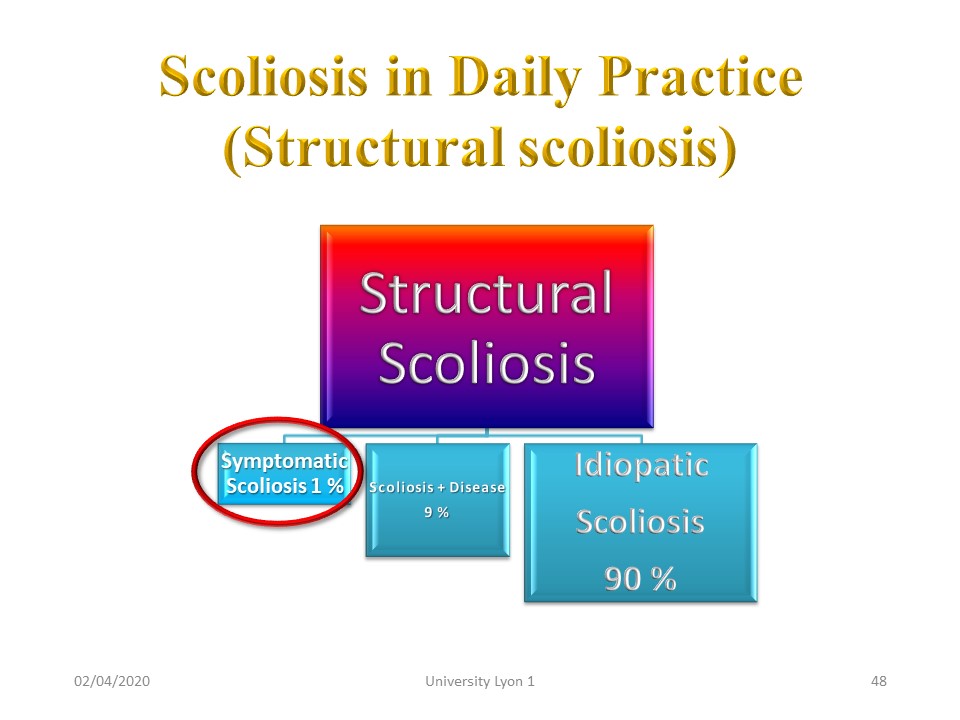
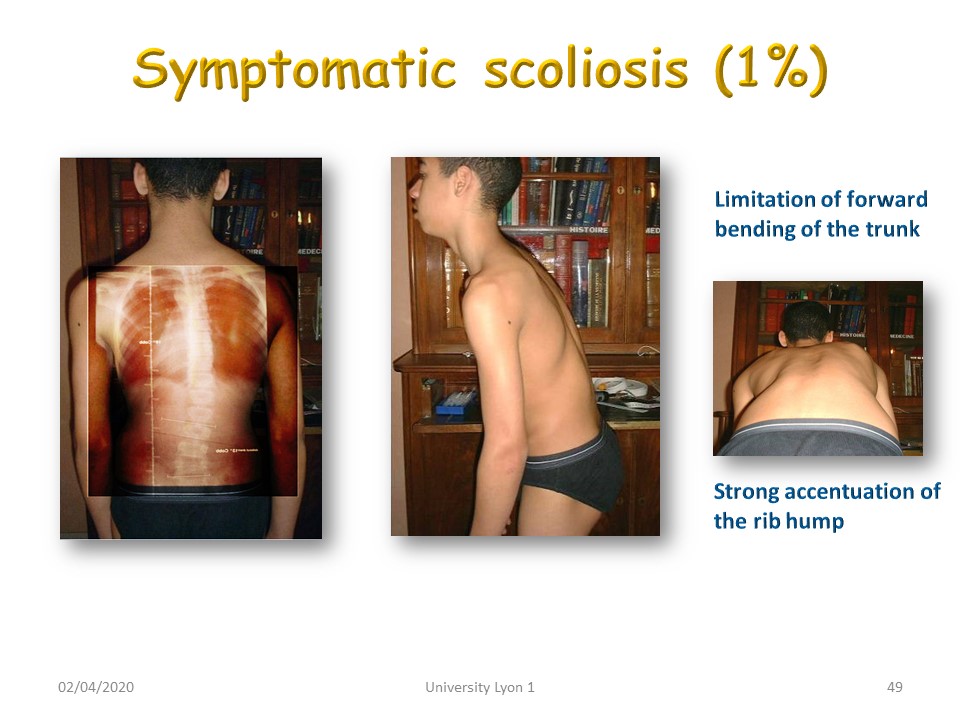
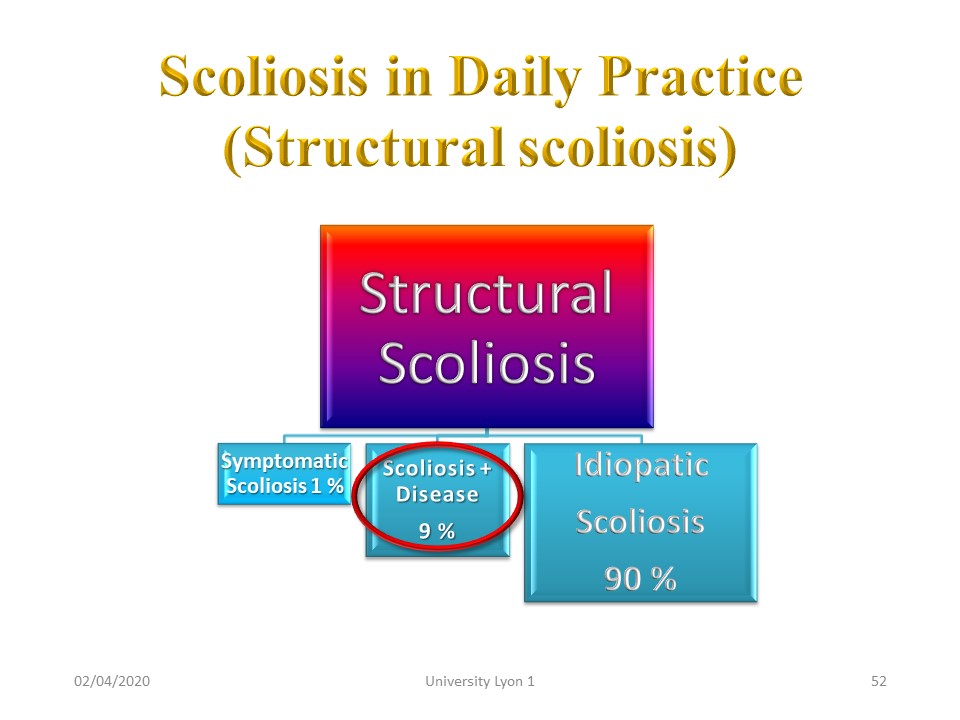
In daily clinical practice, idiopathic scoliosis affects 90% of structural scoliosis. In 10% of cases, scoliosis accompanies an already known disease or will facilitate its diagnosis. In 1% of cases, we will speak of symptomatic scoliosis.
|
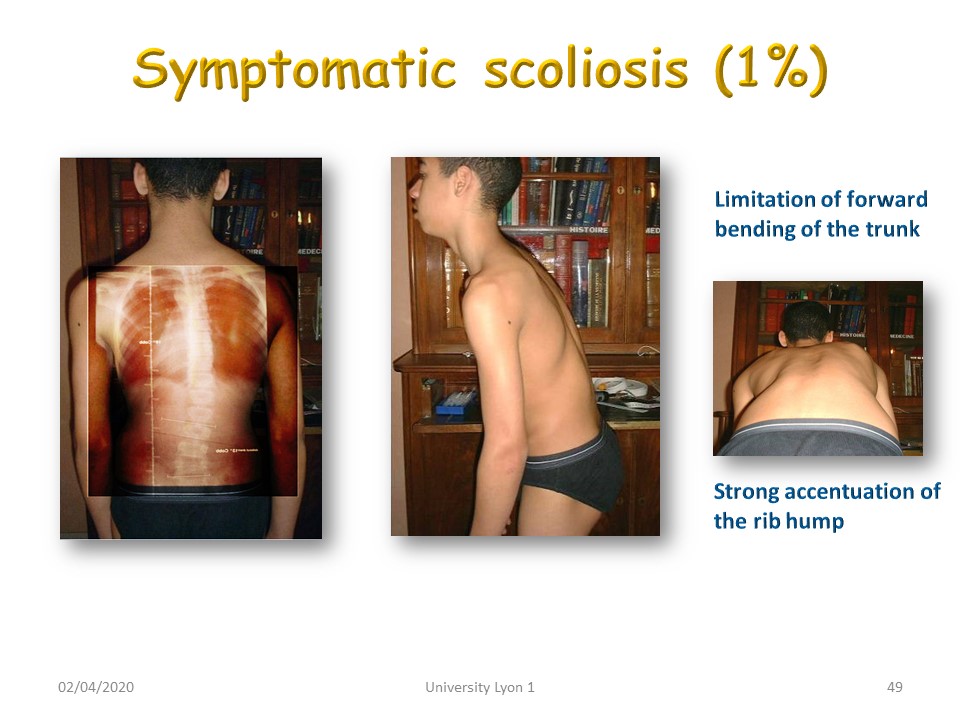 |
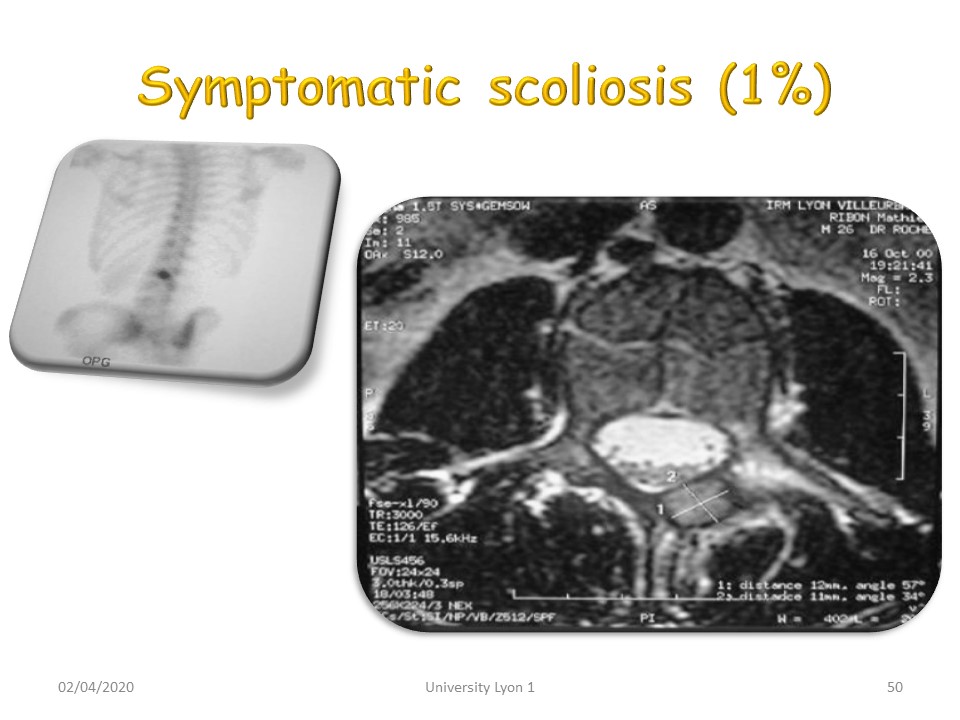
SYMPTOMATIC SCOLIOSIS is characterized by a large curvature with rigidity of the trunk and frequently pain. There is dysfunction with lateral flexion during anterior flexion of the trunk. In this position, the gibbosity is much more accentuated than would be the standing radiological angulation. Complementary examinations, scintigraphy, CT scan, MRI will clarify the etiology.
|
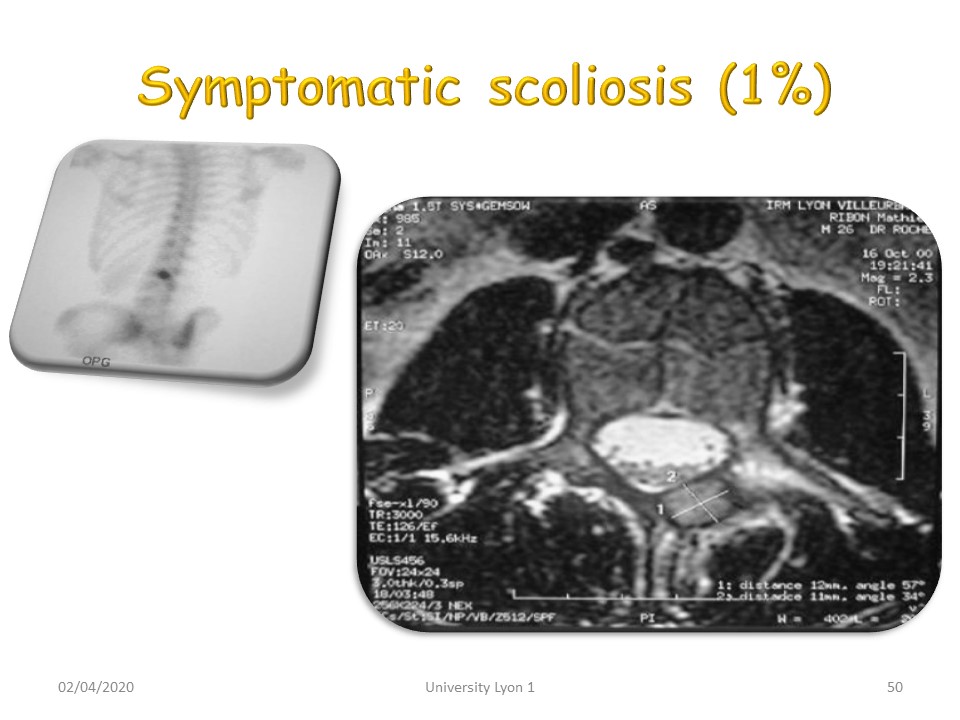 |
It was an osteoid osteoma on the posterior arch of the vertebral body. Formerly the scintigraphy highlighted hyper fixation. Currently the MRI shows the image in central nidus on the posterior lamina.
|
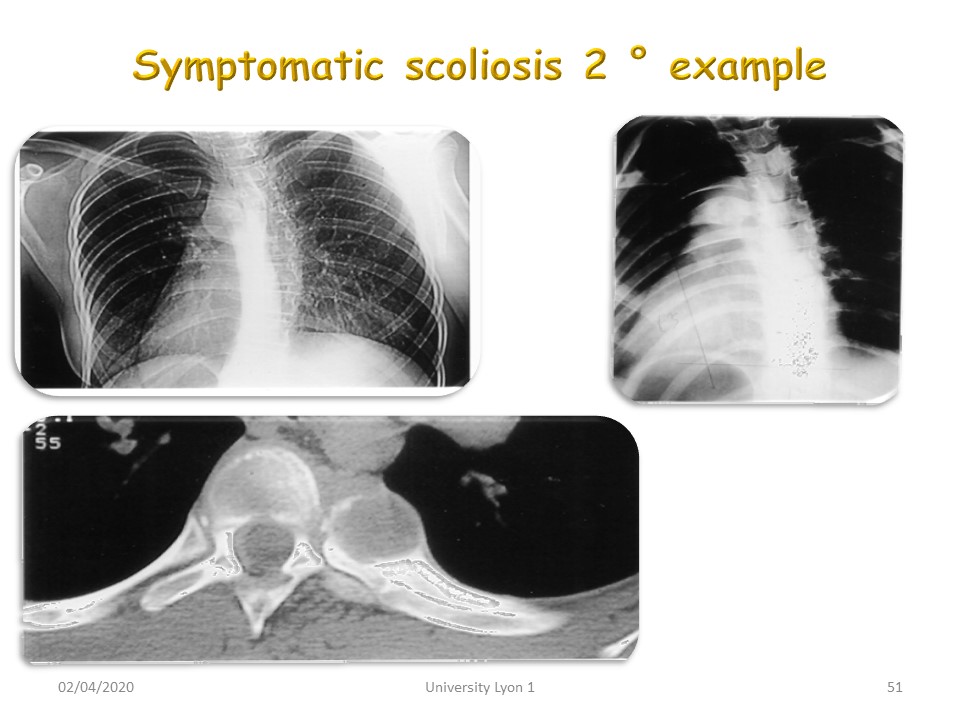 |
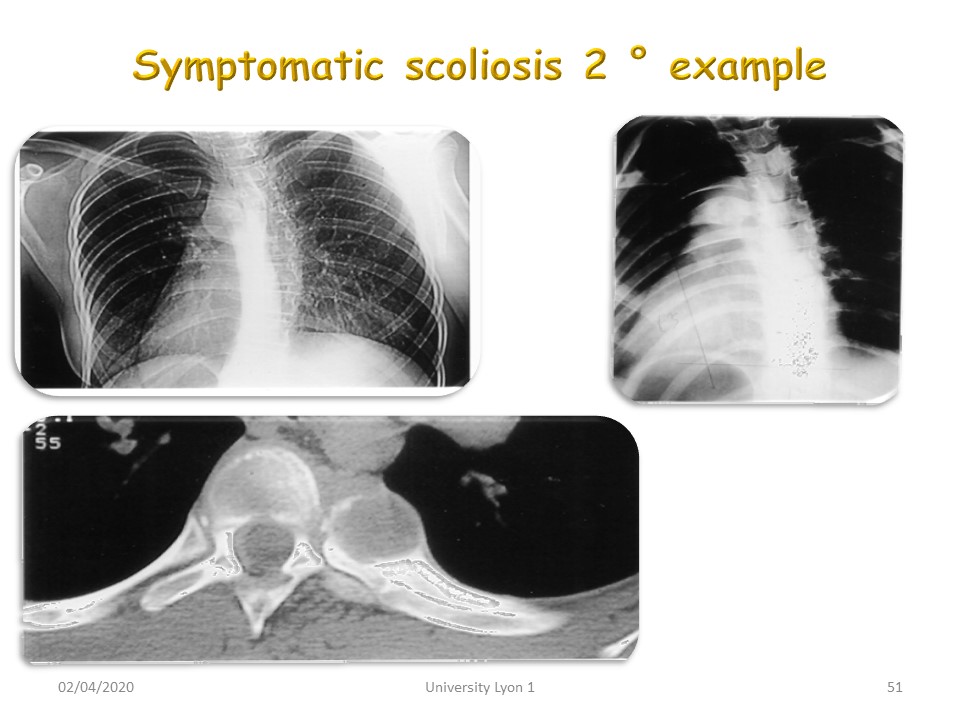
In this case, It was an X histiocytosis near the costo-vertebral joint. The diagnosis was delayed because the tumor was located near the arch of the aorta. It is the persistence of pain under the brace that alerted us.
|
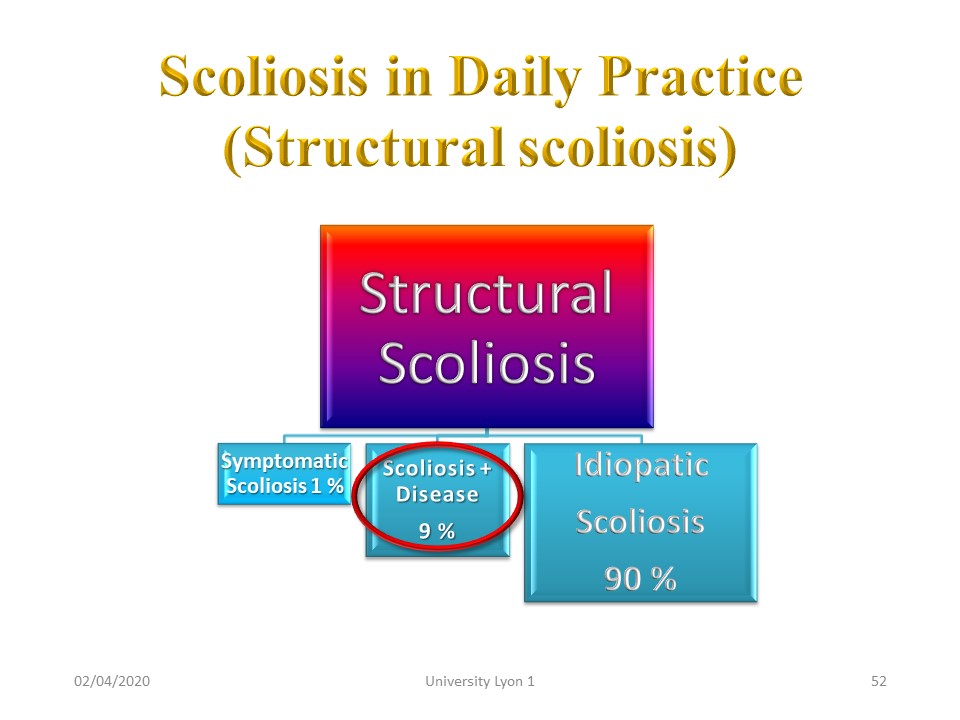 |
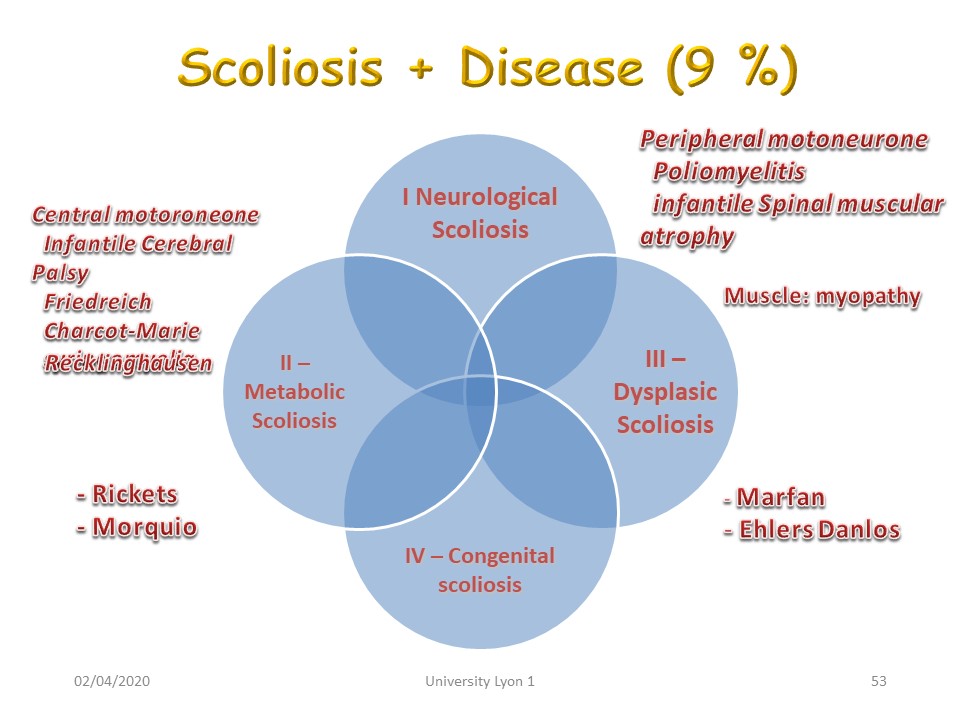
We will now see some of the most common diseases associated with scoliosis.
|
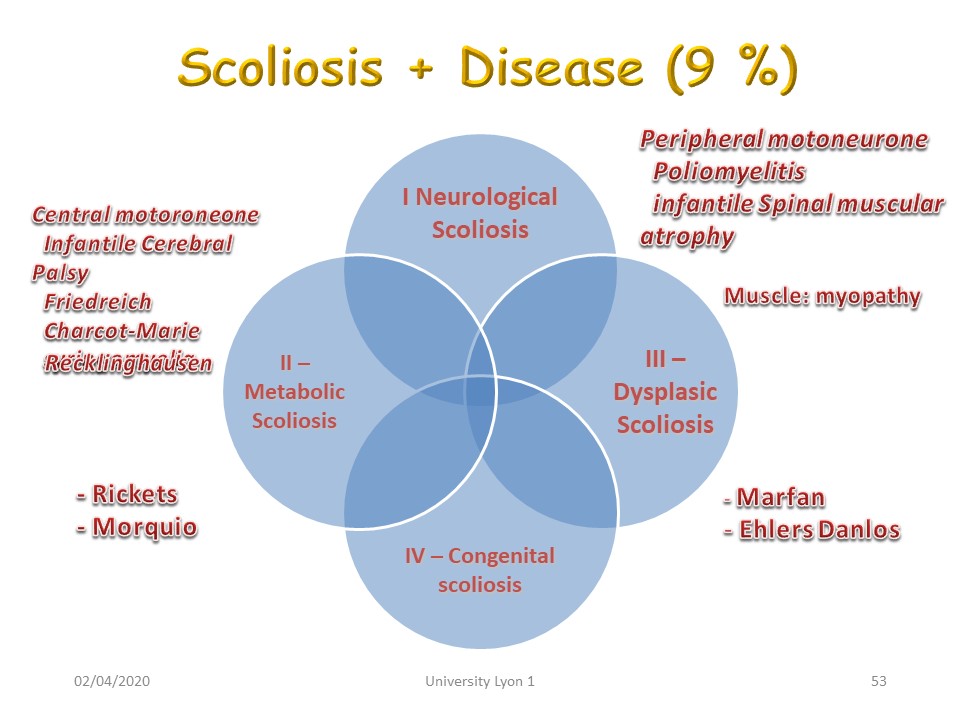 |
The diseases can be grouped into 4 chapters.
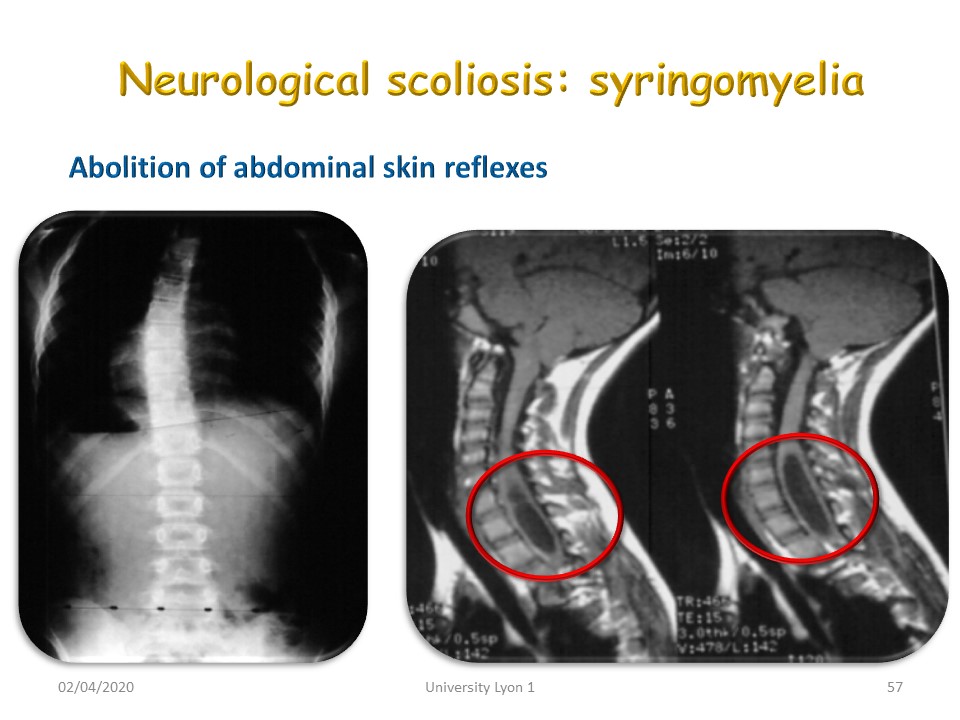
1. Neurological scoliosis with central motor neuron involvement. Cerebral palsy. Friedreich. Charcot-Marie. Syringomyelia. Recklinghausen. Peripheral motor neuron involvement is achieved in: Poliomyelitis. Infantile Spinal muscular atrophy.
2. Metabolic diseases such as rickets and Morquio's disease.
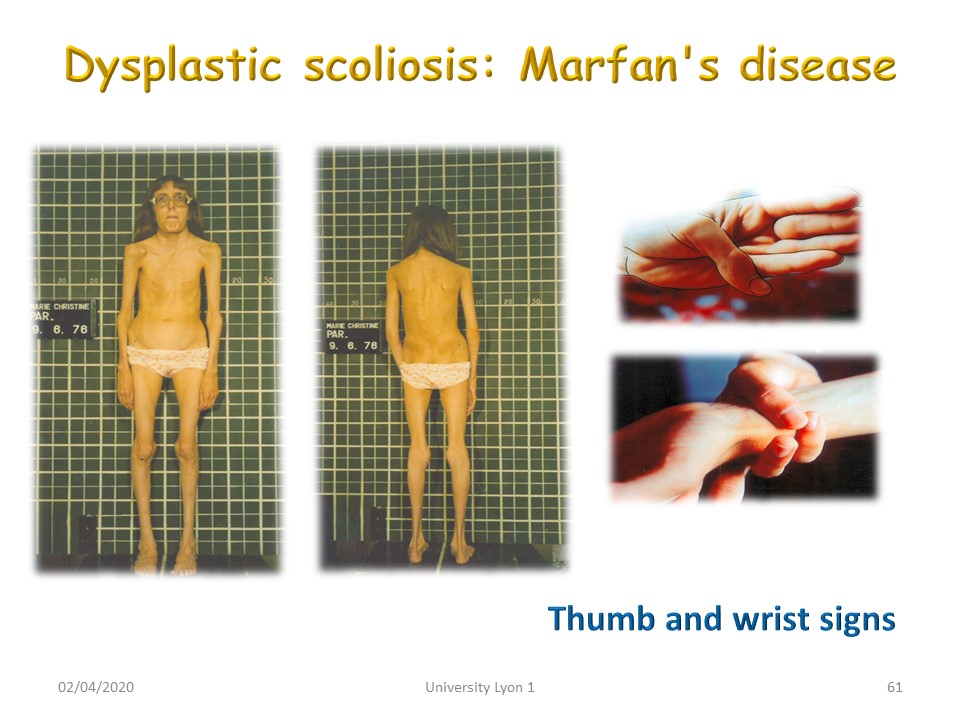
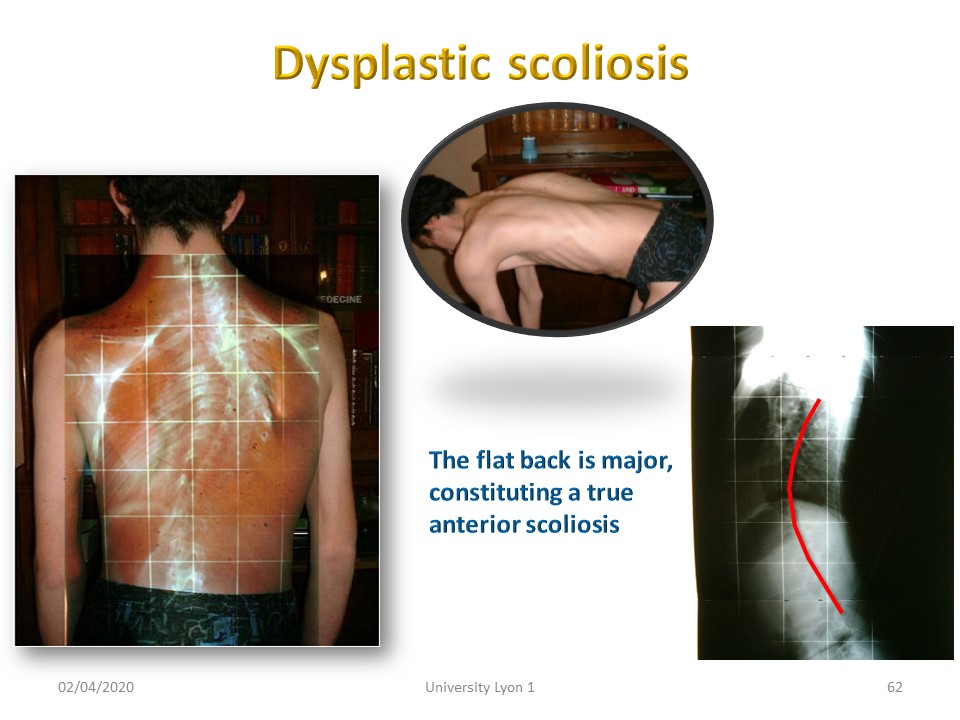
3. Dysplastic scoliosis such as Marfan's disease or Ehlers Danlos.
4. Congenital scoliosis
|
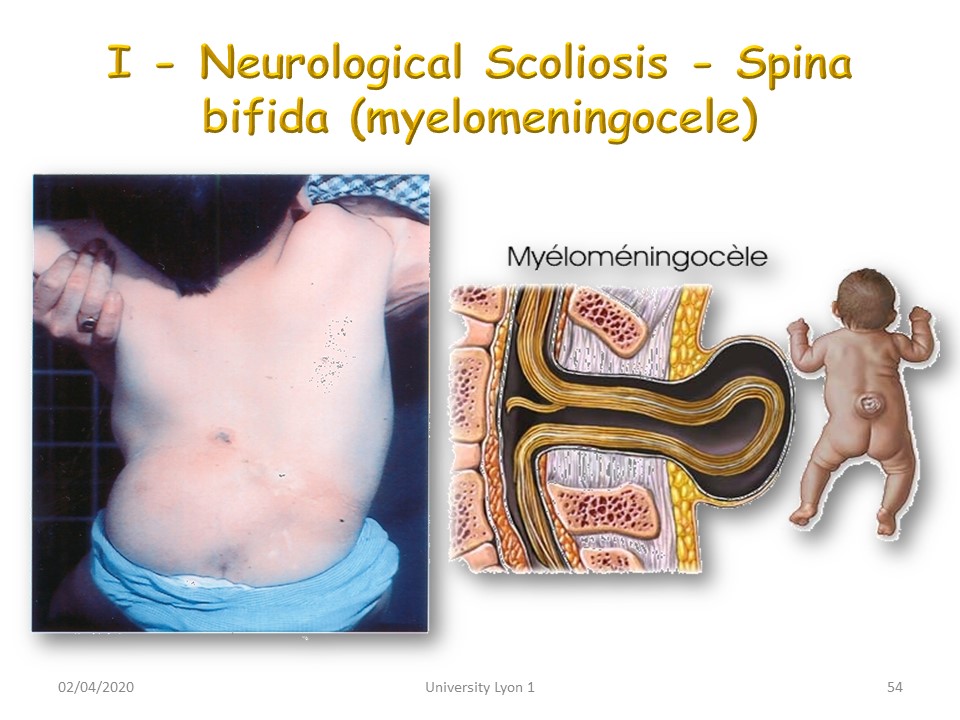 |
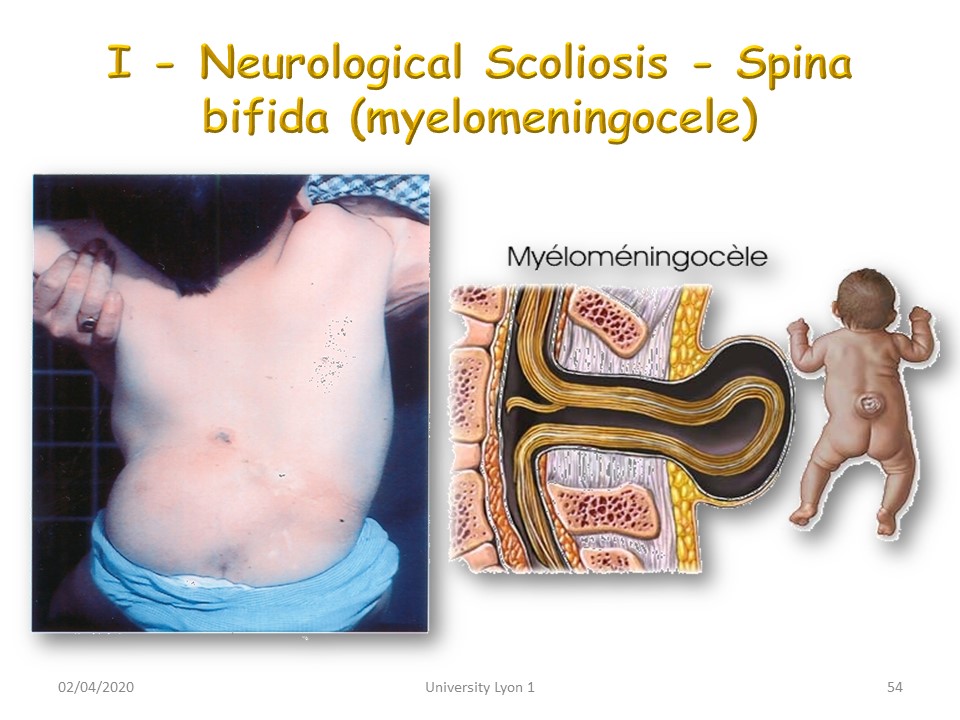
Spina bifida are currently less common. Scoliosis is often associated with an imbalance in paravertebral muscle involvement.
|
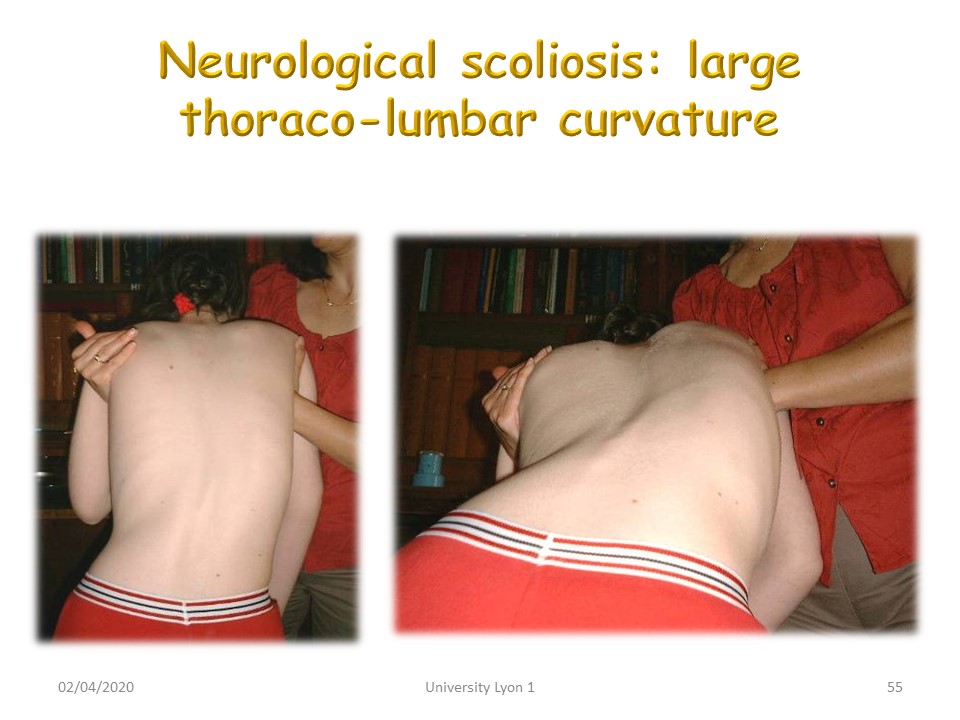 |
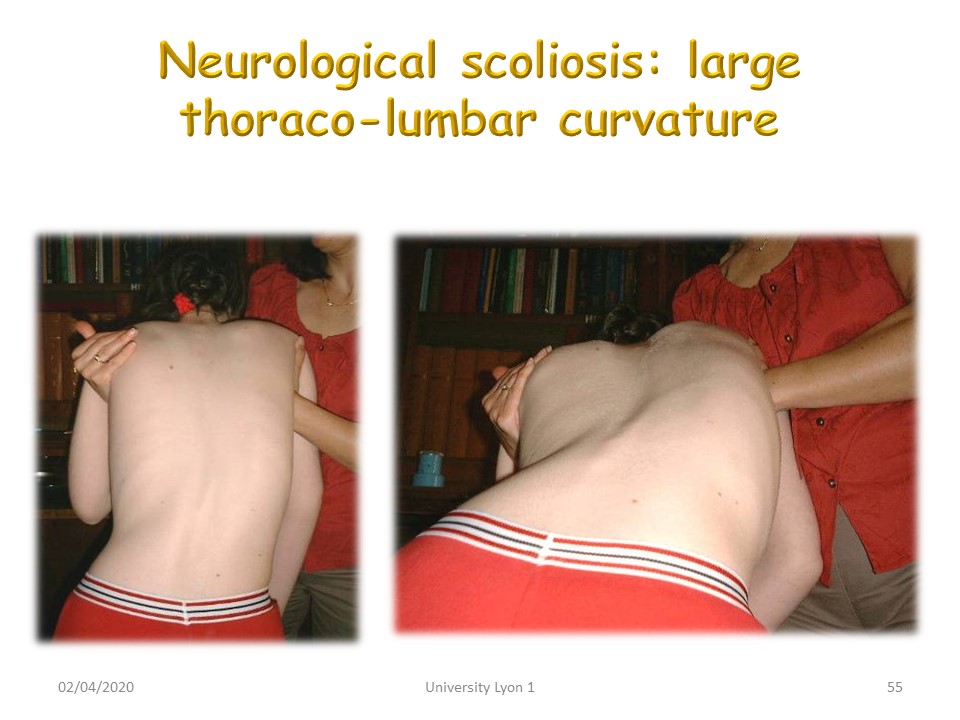
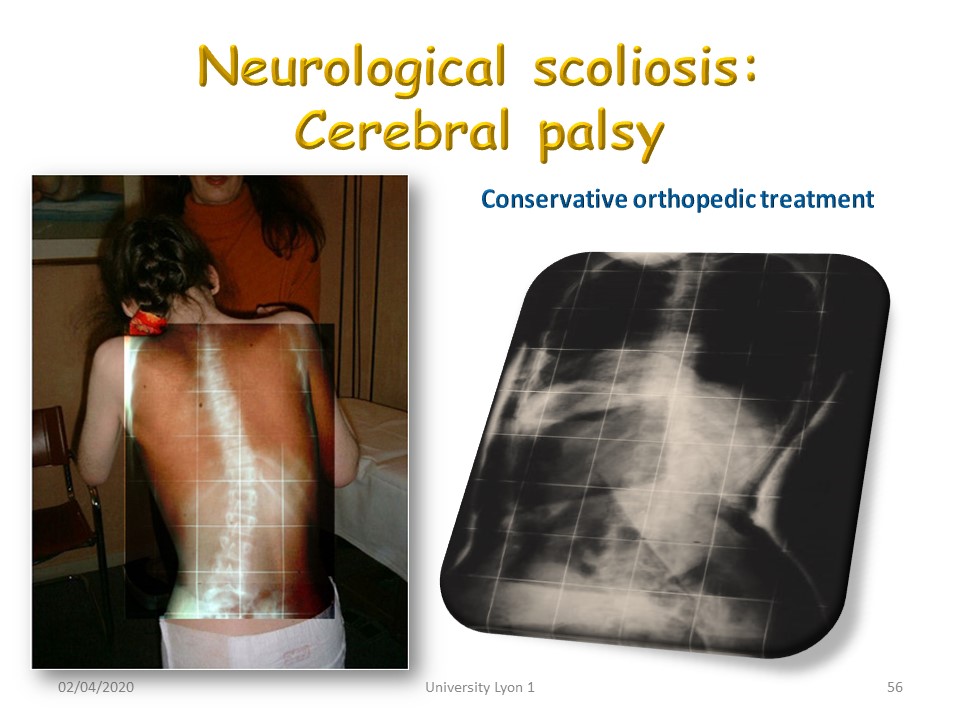
The neurological disease is most often known, as in this child with cerebral palsy. The thoraco-lumbar curvature is large radius. Reducibility will depend on spasticity. The braces are difficult to achieve. when the children are walking. The instant molding in a few seconds is an advantage for the realization of corrective braces. When the children are in wheelchairs, one can make a molded seat during the day and a hyper-corrector brace during the night.
|
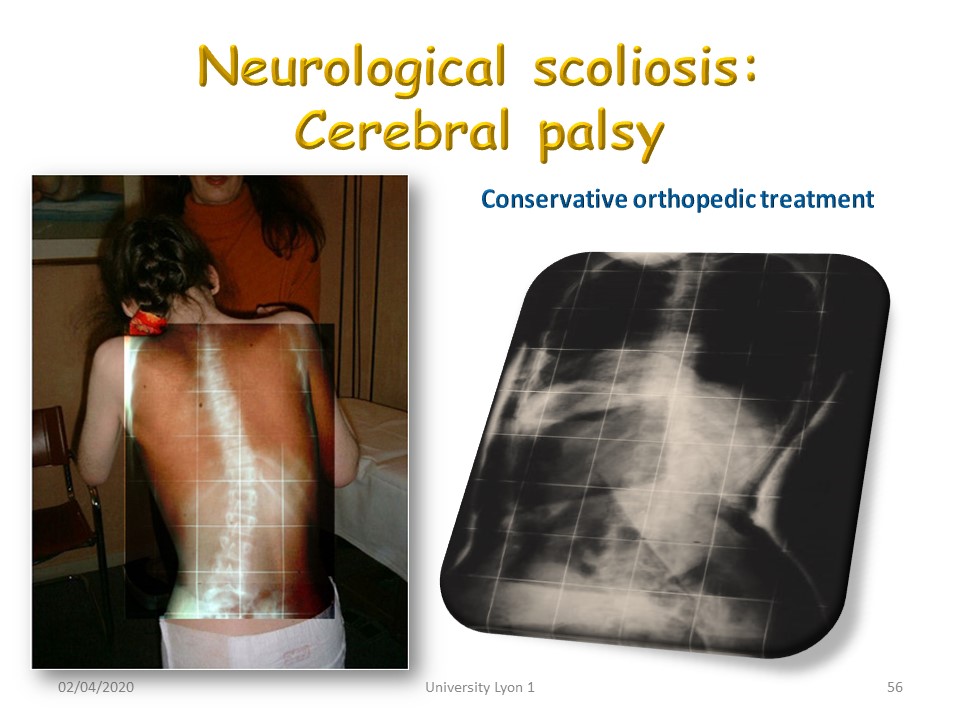 |
In this child we were able to make a plaster cast and a classic Lyon brace that was well tolerated.
|
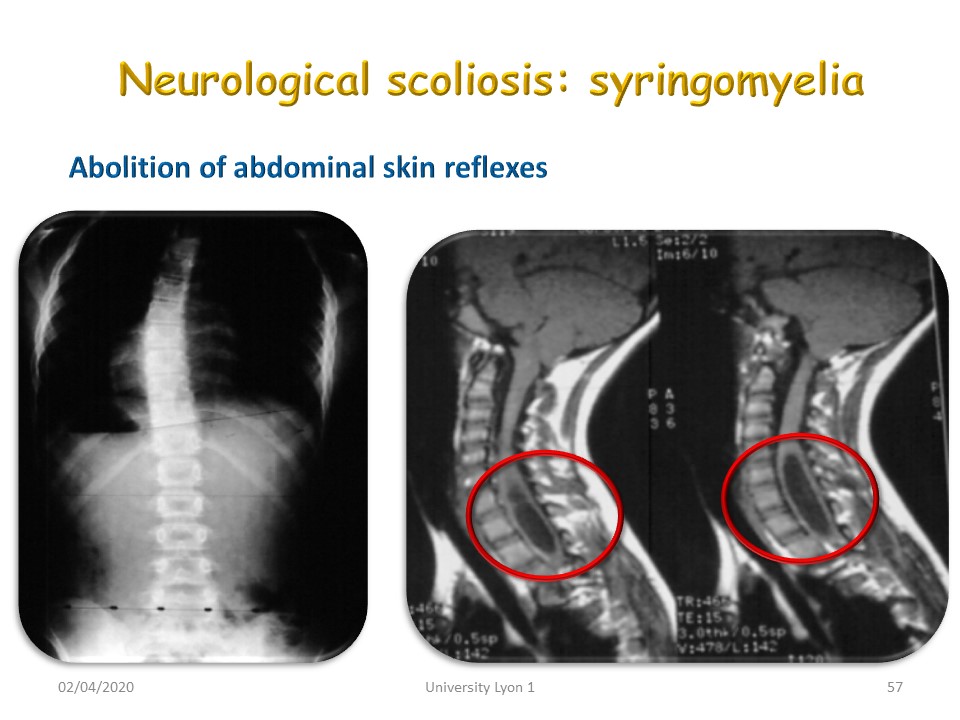 |
We have already mentioned Chiari malformation and syringomyelia. After puberty, pressure is restored in the cerebrospinal fluid and a bypass is not necessary.
|
 |
Dystonic scoliosis is similar to spasmodic torticollis. Curvatures are unreal, often completely unbalanced.
|
 |
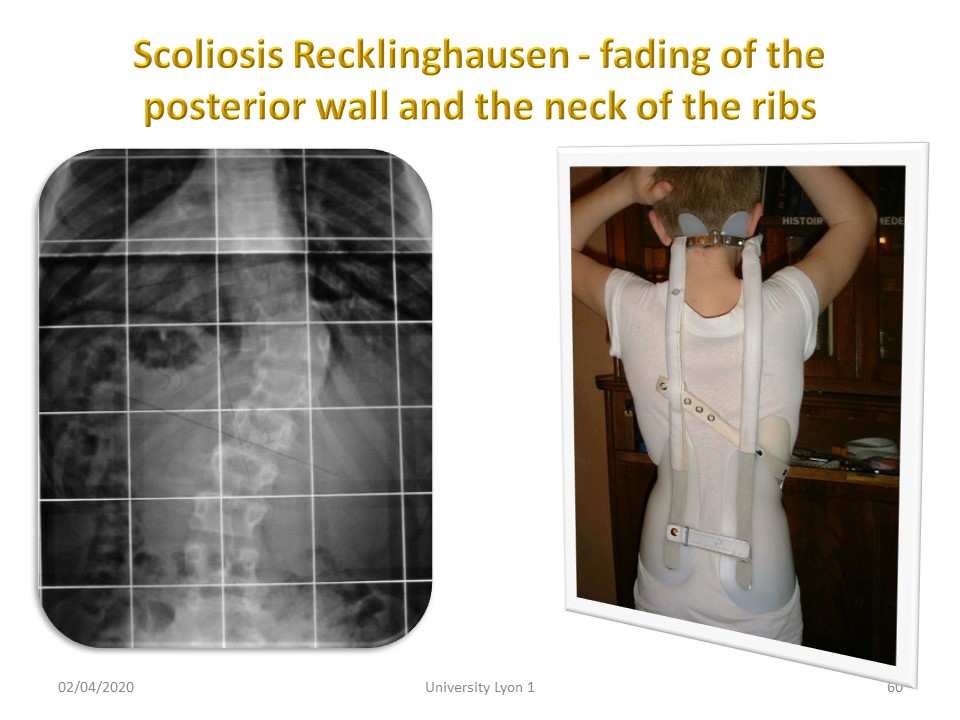
Recklinghausen's disease is a phacomatosis and affects the tissues derived from the ectoderm. The presence of more than 7 café au lair spots is characteristic.
|
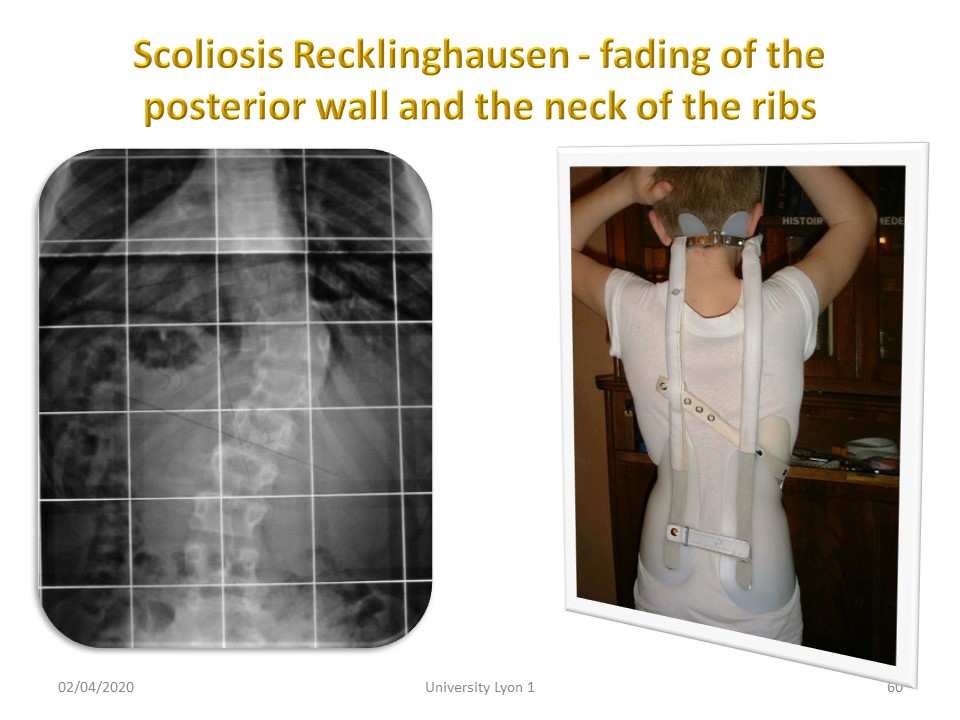 |
Scoliosis involves a diminution of the posterior wall of the vertebral body and the neck of the ribs, the embryology of which derives from the ectoderm. This narrowing widens the medullary canal and avoids neurological complications. The posterior arch remains intact, which limits the extension. Curvatures are short and make it difficult to brace.
|
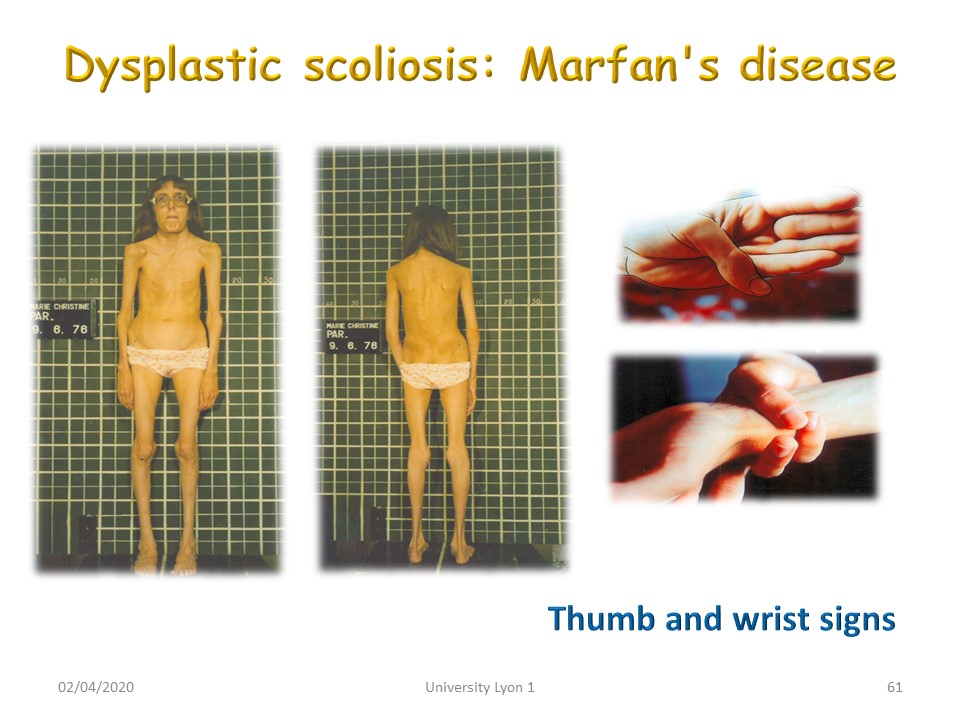 |
Marfan's disease sometimes has scoliosis. Clinically hyperlaxity is noted by the thumb and wrist tests. When requesting adduction of the thumb, the pulp largely exceeds the ulnar edge of the hand reflecting hyperlaxity. When the opposite wrist is surrounded by the thumb and the 5th finger: the pulps overlap, reflecting dolichostomelia. Scoliosis is treated as idiopathic scoliosis, seeking to correct the associated thoraco-lumbar kyphosis.
|
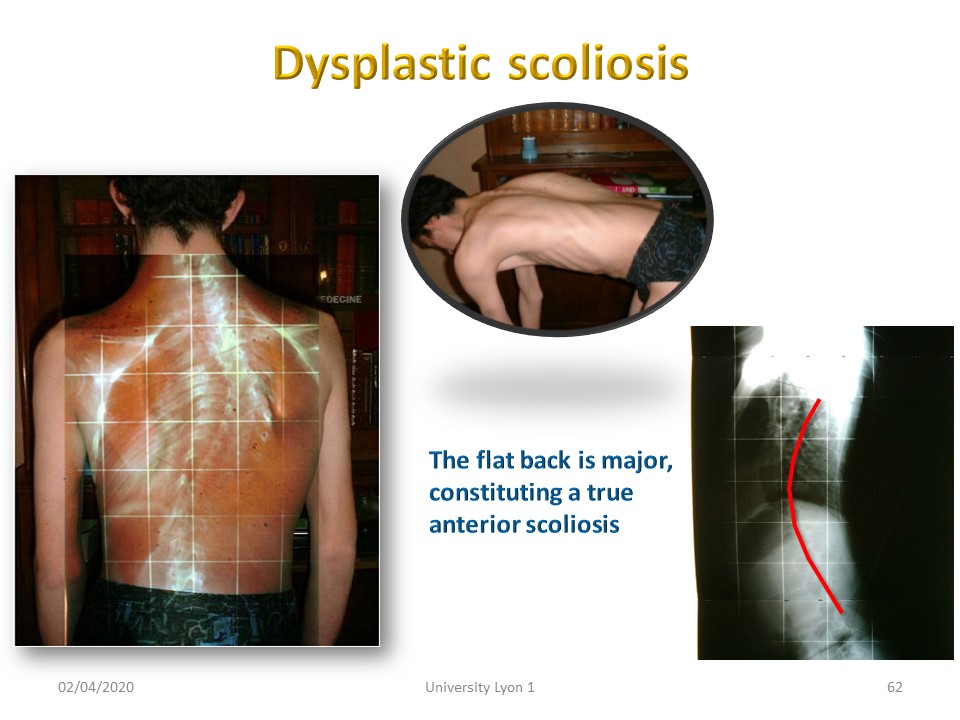 |
Dysplastic scoliosis has an angular gibbosity making it very difficult conservative orthopedic treatment and a major flat back.
|
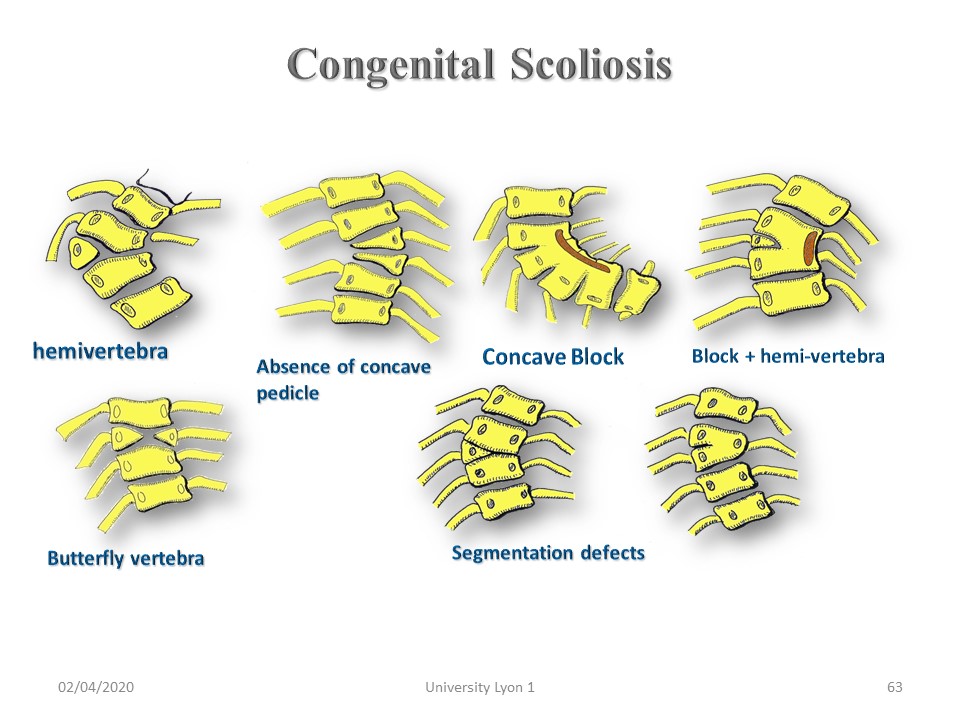 |
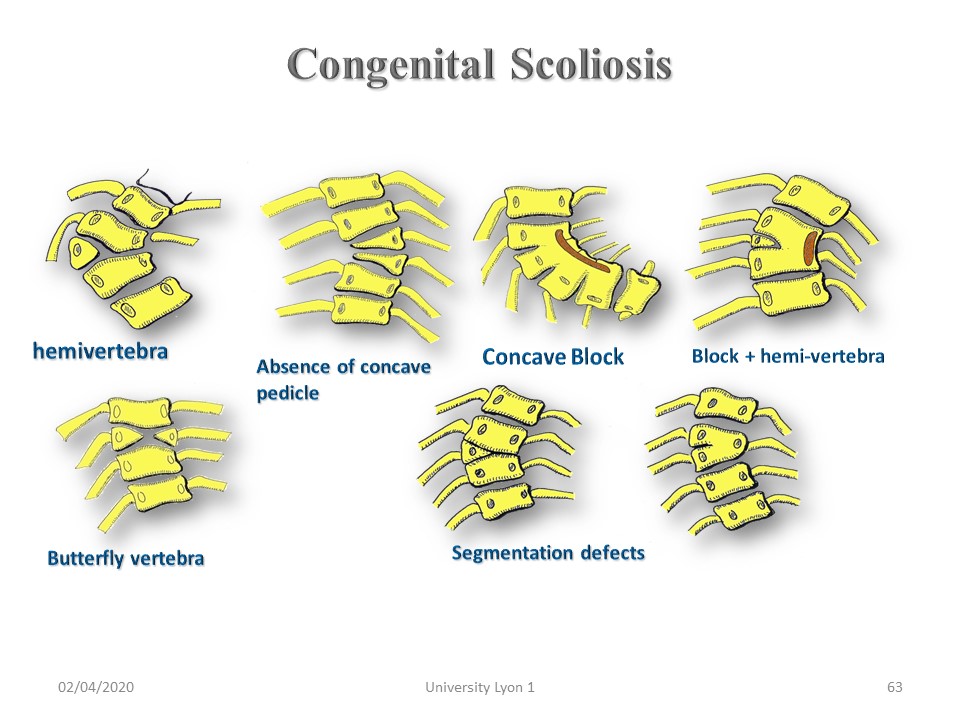
Scoliosis by congenital vertebral malformation is constituted the 4th week of pregnancy. It is associated in one third of the cases with renal and cardiac malformations. Most often there are unilateral segmentation defects with partial blocks. The most serious malformation is the hemi vertebra especially when isolated. The most common malformation is the butterfly vertebra. There is no correlation between the radiological aspect and the progressive prognosis due to the lack of visibility of the growth cartilage. The future is played out in the first two years of life, when one may have to perform a surgical epiphysiodesis. Past this milestone, the Milwaukee Night Orthosis guides growth and stabilizes scoliosis.
|
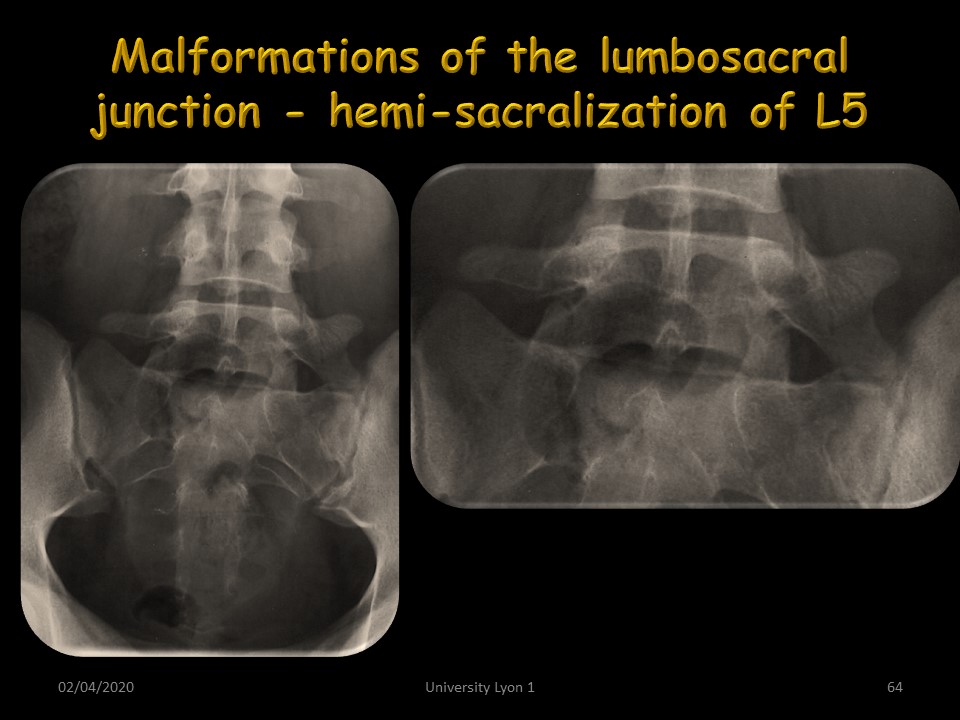 |
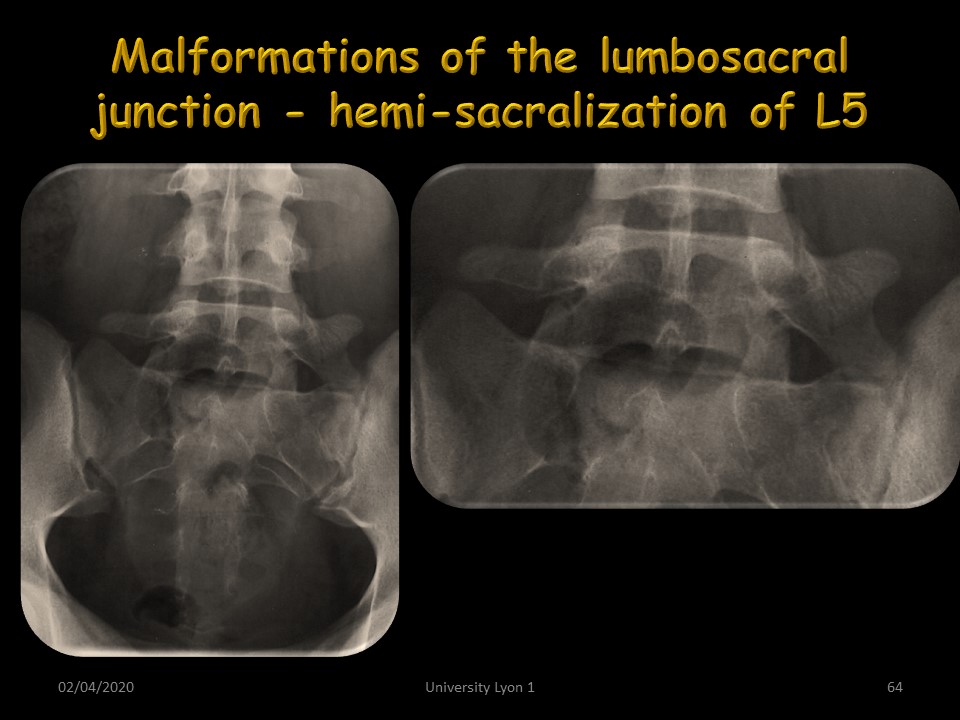
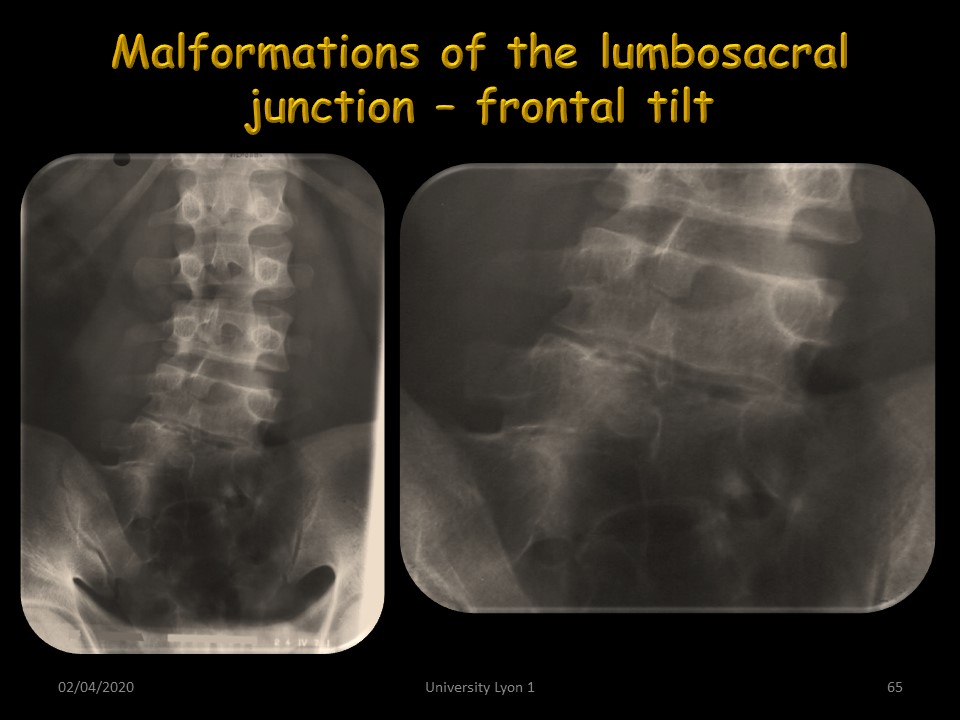
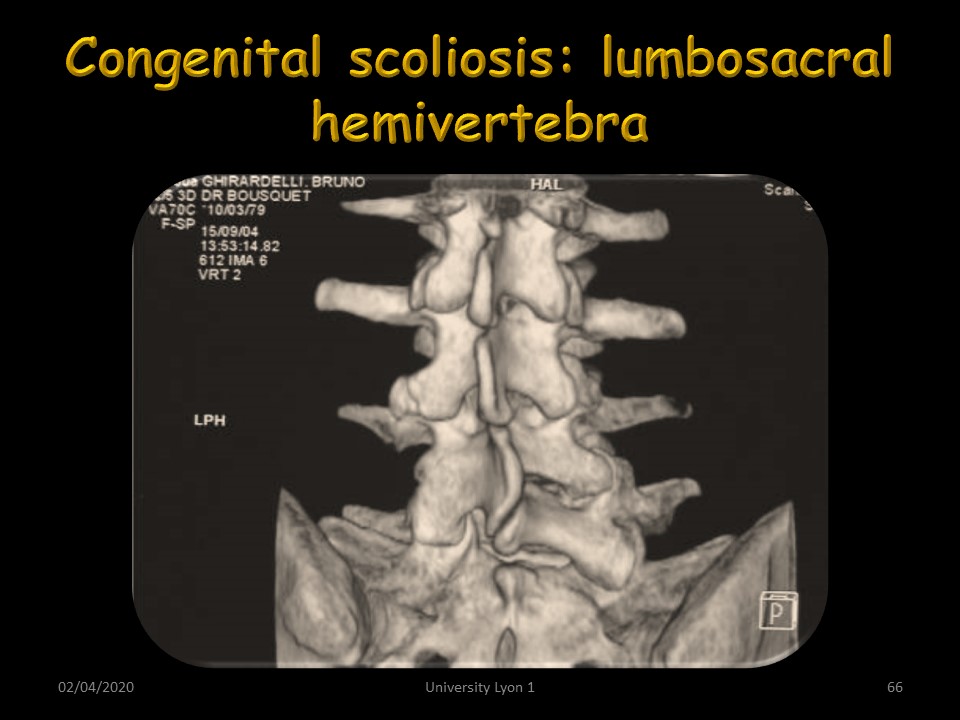
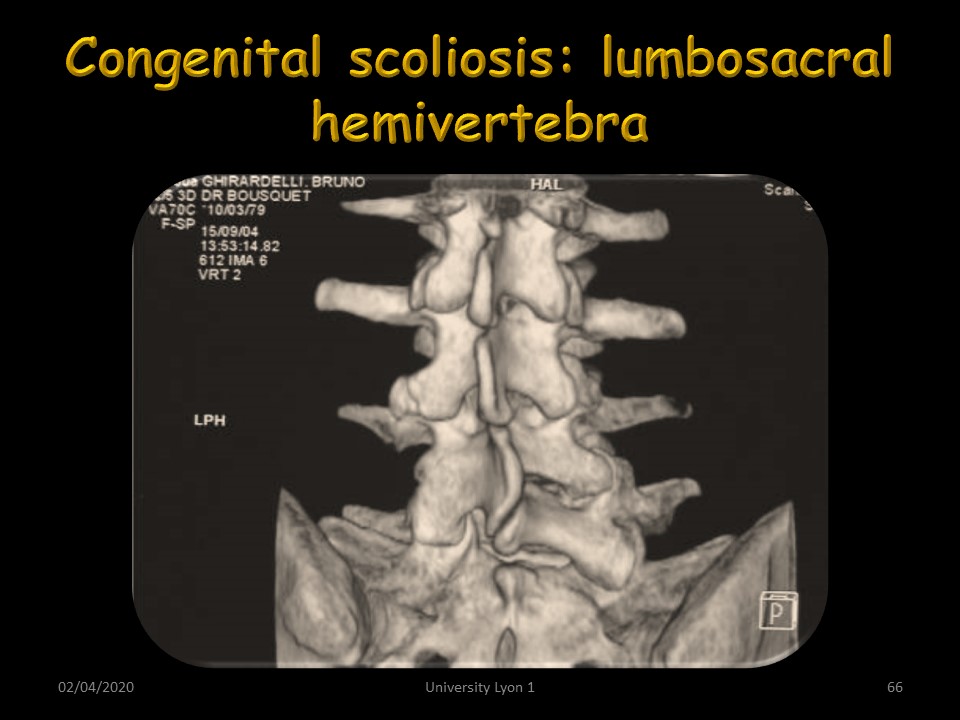
At the level of the lumbosacral junction, a transitional vertebra with for example hemi-sacralization of L5 can cause lumbar scoliosis with frontal tilt. The frontal tilt is even more obvious when there is a L5 hemivertebra. Three-dimensional CT reconstruction is useful for visualizing malformation.
|
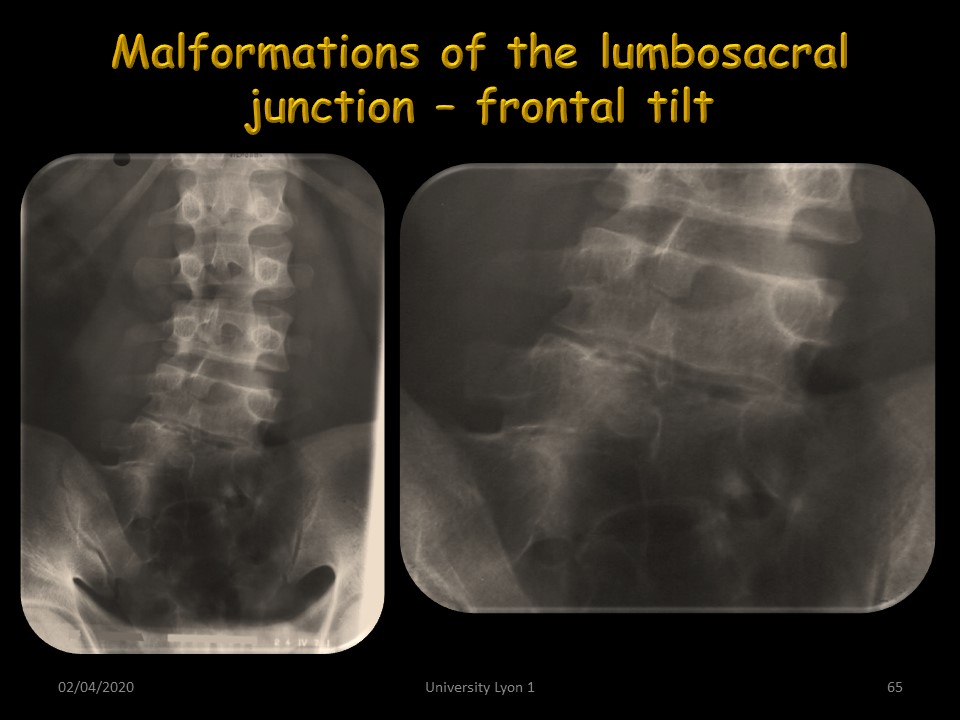 |
This is the case of this malformation with significant obliquity of the upper plate of L5
|
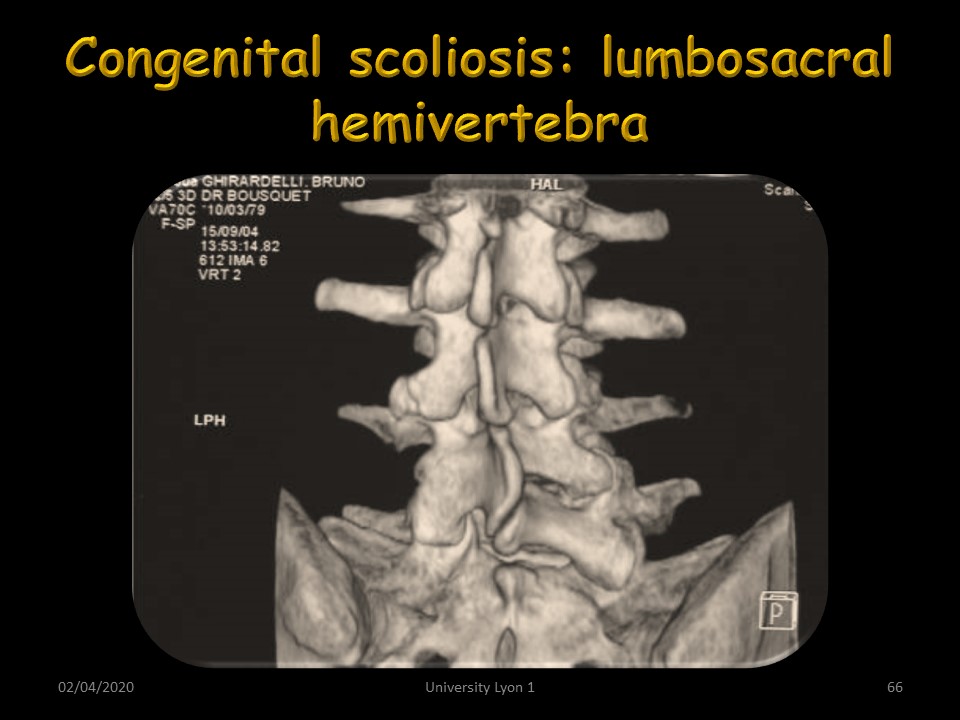 |
The 3D reconstruction by the CT confirms the extra pedicle on the left.
|
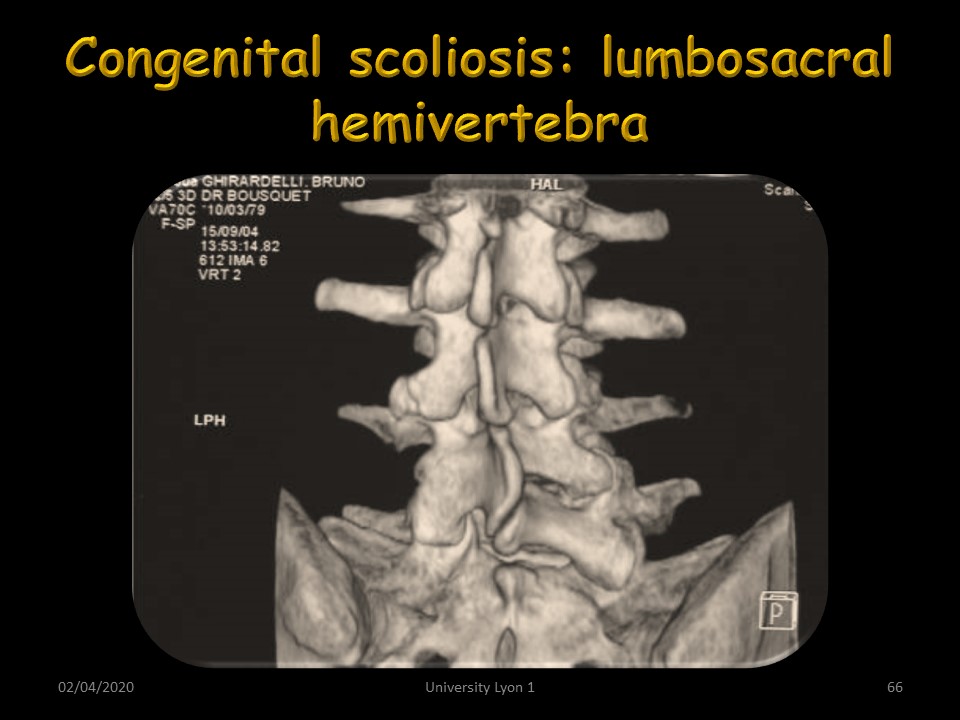 |
The 3D reconstruction by the CT confirms the extra pedicle on the left.
|
 |
|
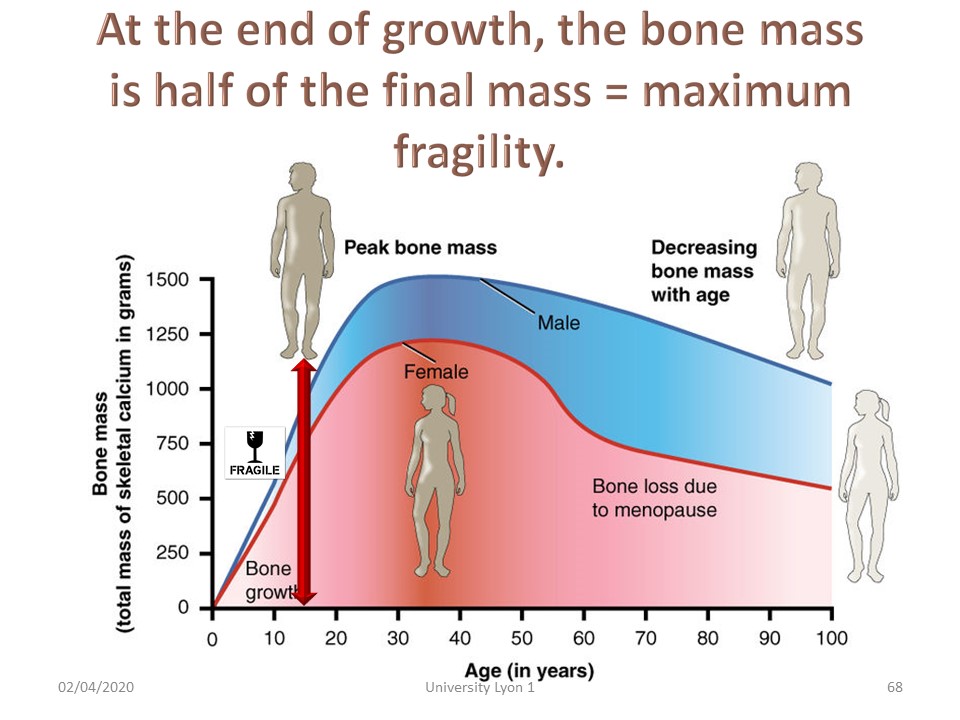 |
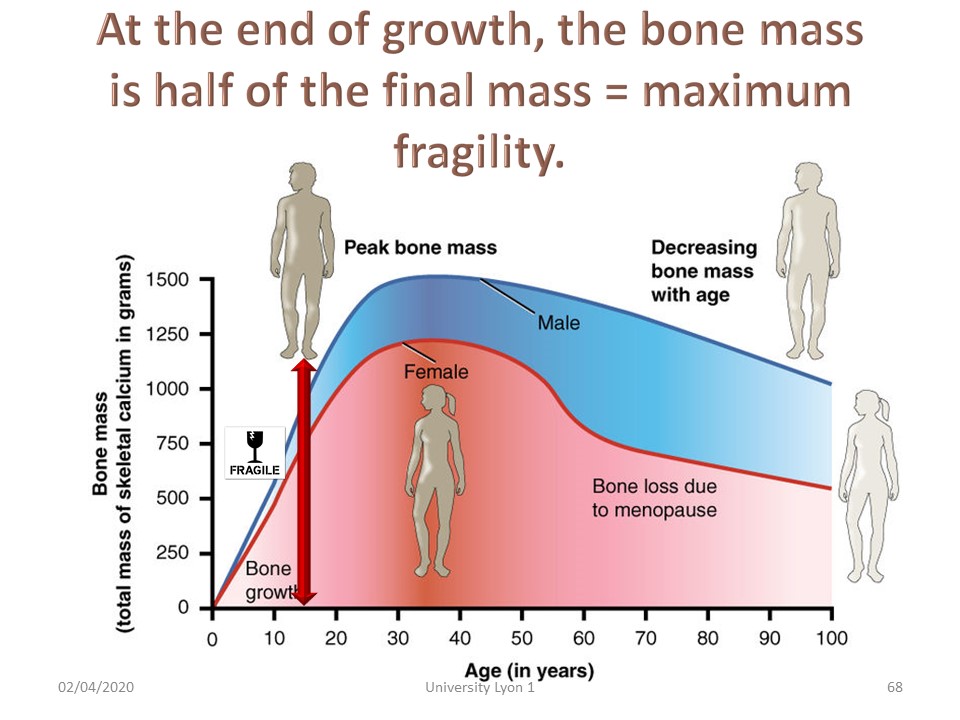
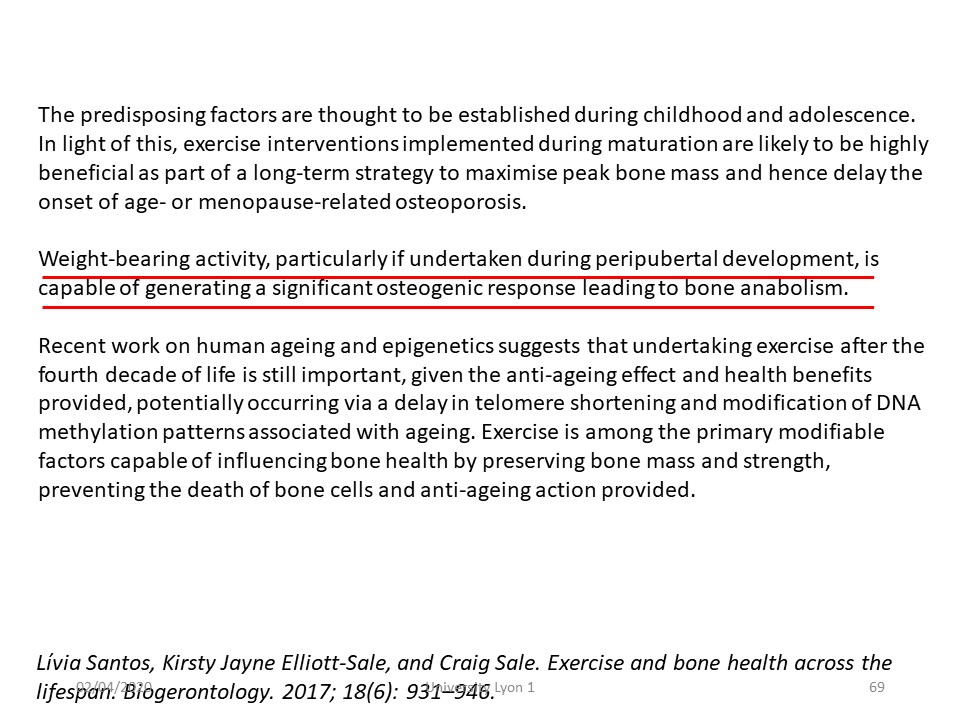
The end of growth in height is the period of maximal bone fragility of scoliosis and for the most important scoliotic curvatures, it is necessary to extend the wearing of the brace.
|
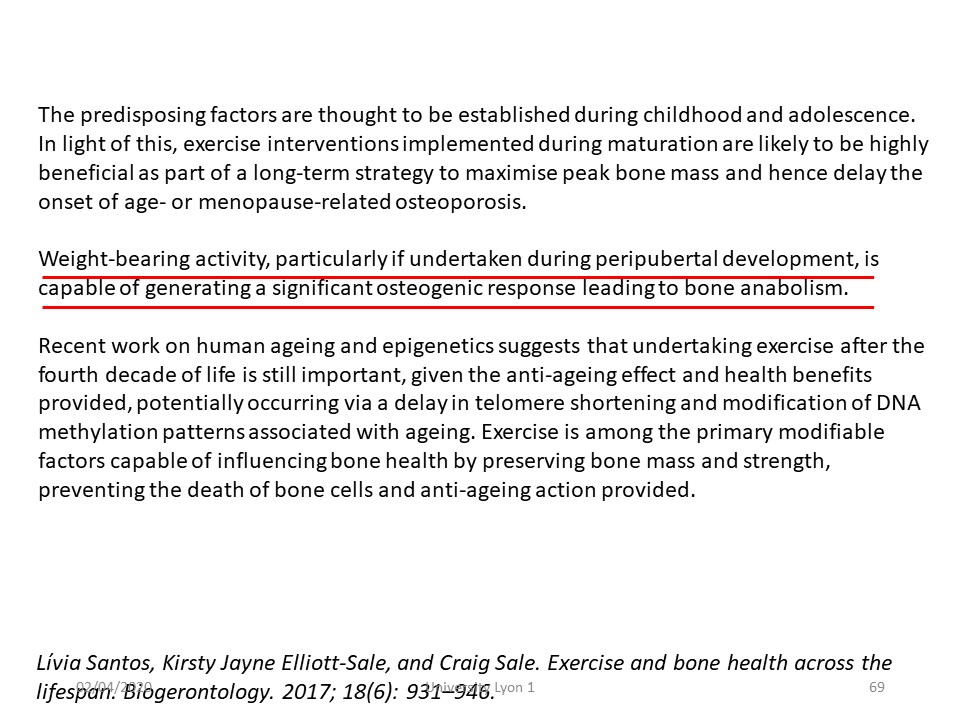 |
In addition to the calcium-rich diet, the axial impact must be associated with the reinforcement of the spiral chains and the weight bearing activities can be advised.
|
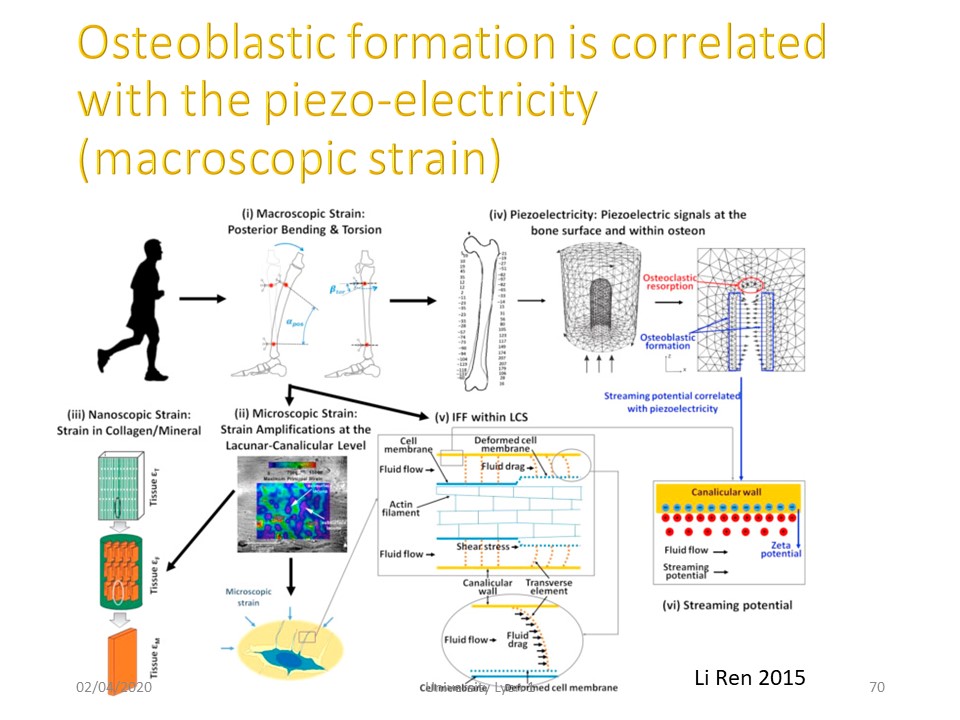 |
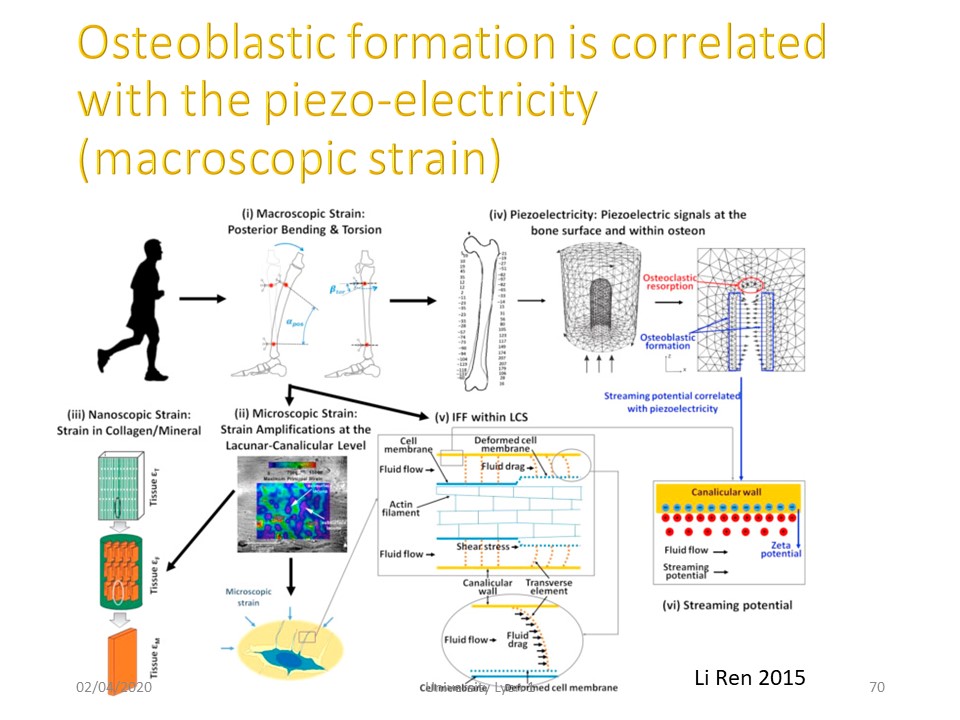
Indeed the mechanical energy of the heel on the ground is transmitted at the level of the spine and creates a piezo-electric current that promotes the fixation of calcium on the bone.
|
 |
Jogging & running at this age combine strengthening of bone mass and spiral chains.
|
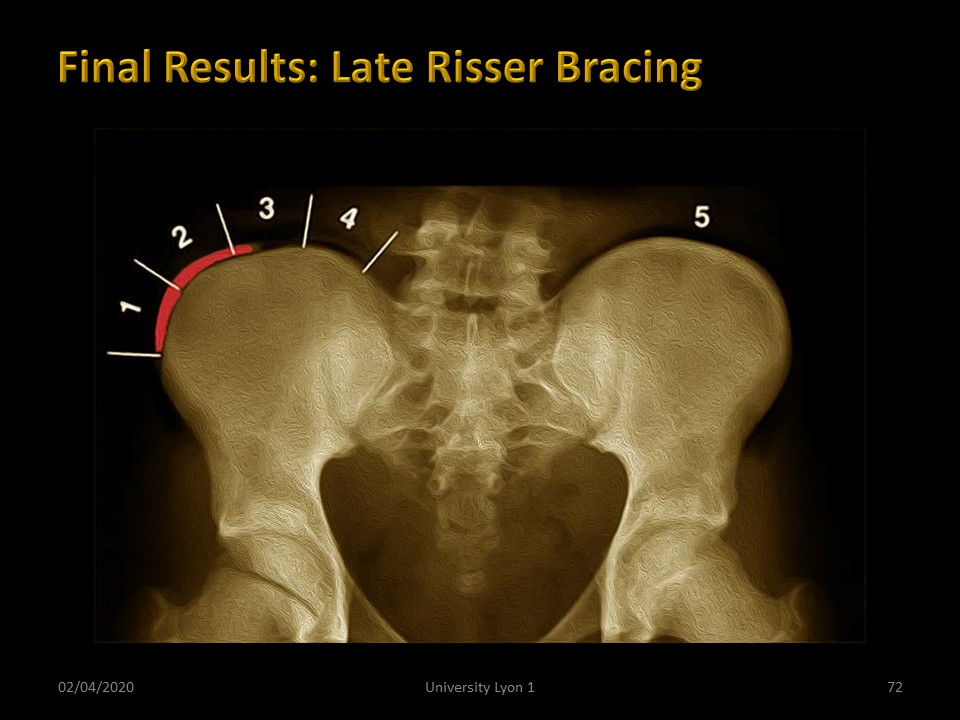 |
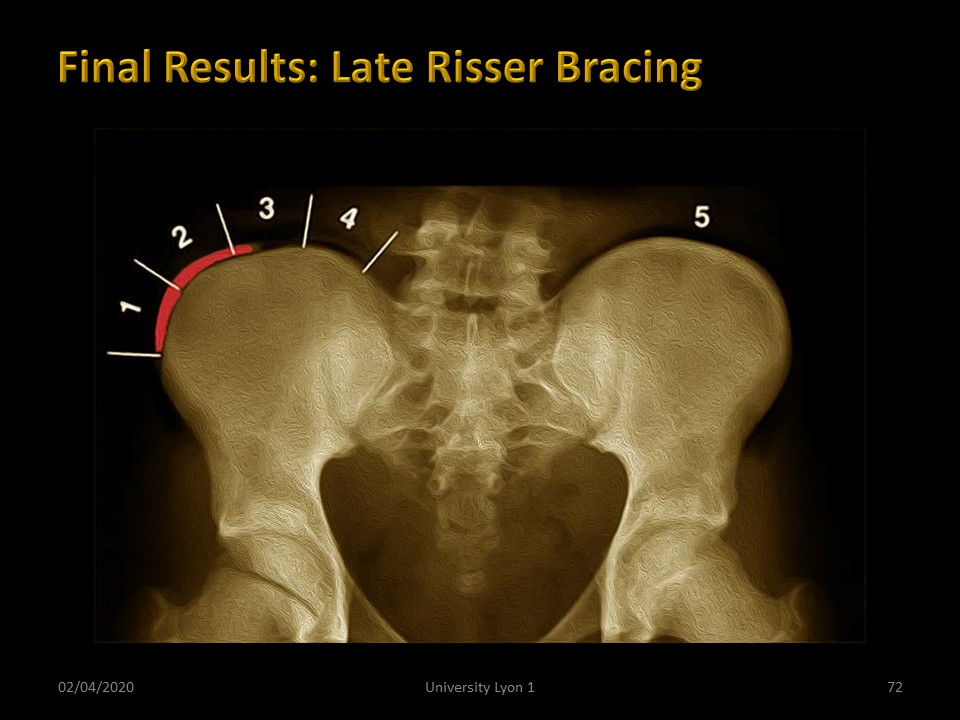
The Lyon method is perfectly adapted to the treatment of scoliosis after Risser 2, because the plastic deformation allows a correction at the level of the soft tissues.
|
 |
The realization of the plaster cast in the past and currently the "full time" wearing of the ARTbrace allow to readjust the tensions along the spine in the maximum corrective position.
|
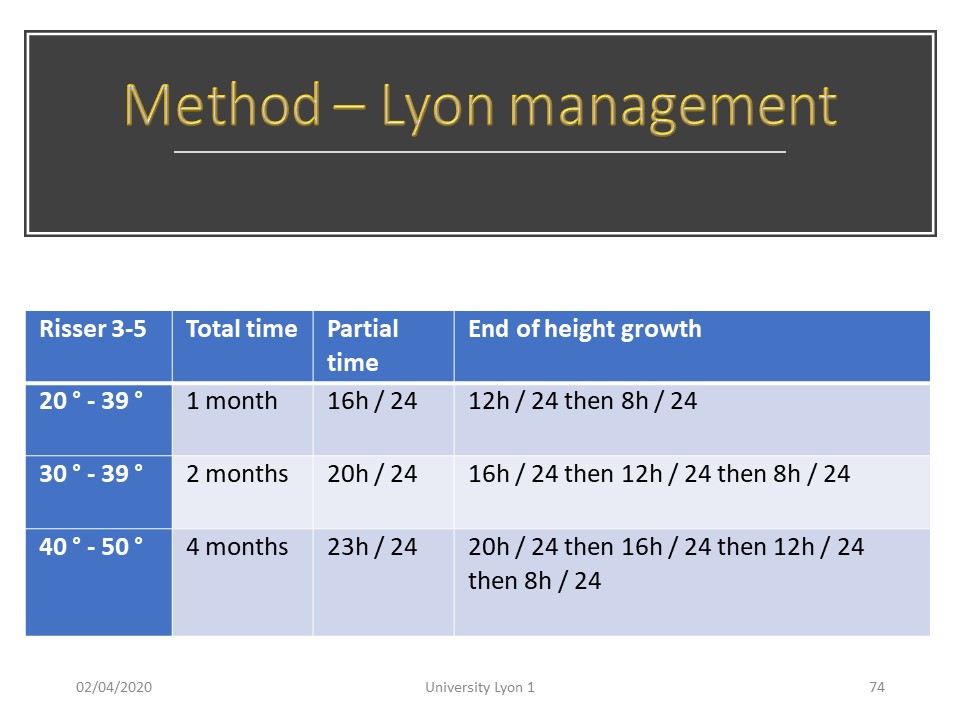 |
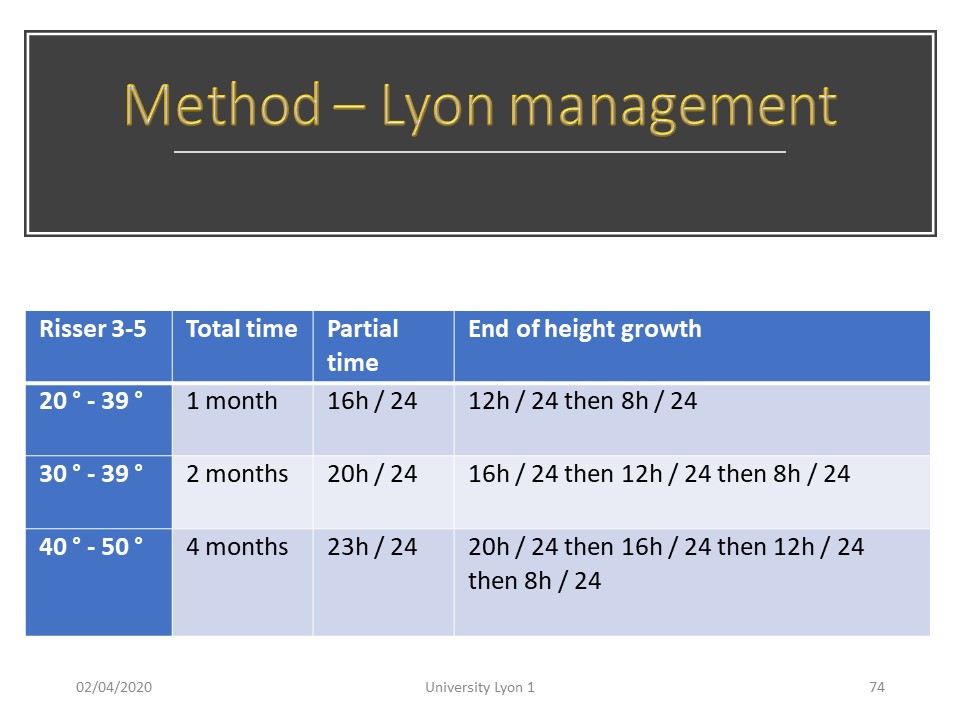
The management remained the same with total time from 1 to 4 months depending on the angulation of the scoliosis. In the same way, the part-time port with progressive removing of 4 hours per day every 6 months makes it possible to standardize the protocol from the first consultation.
|
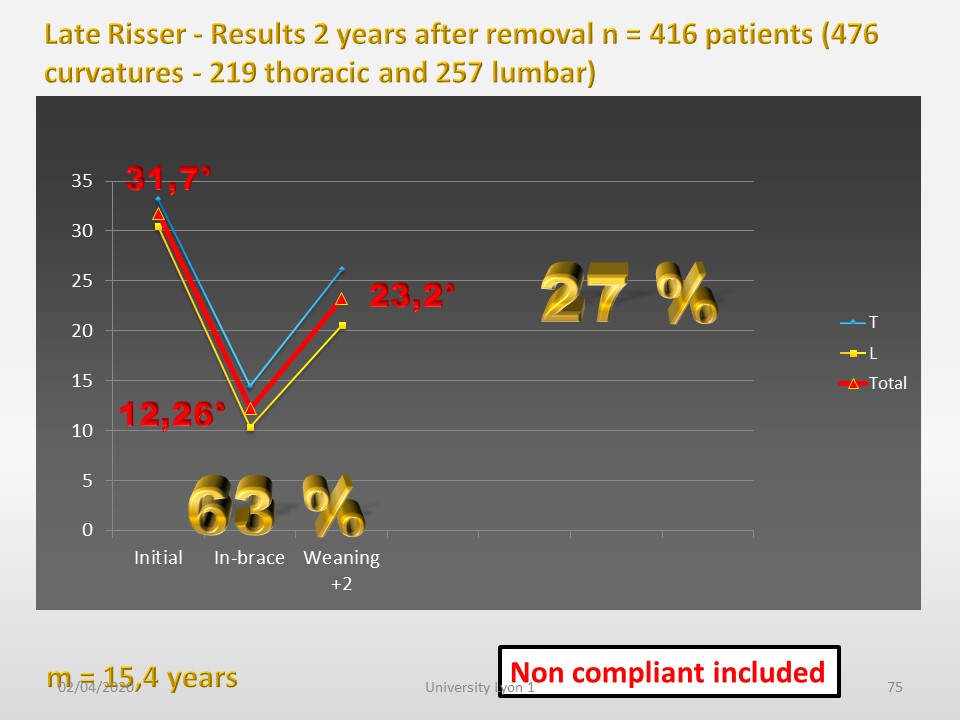 |
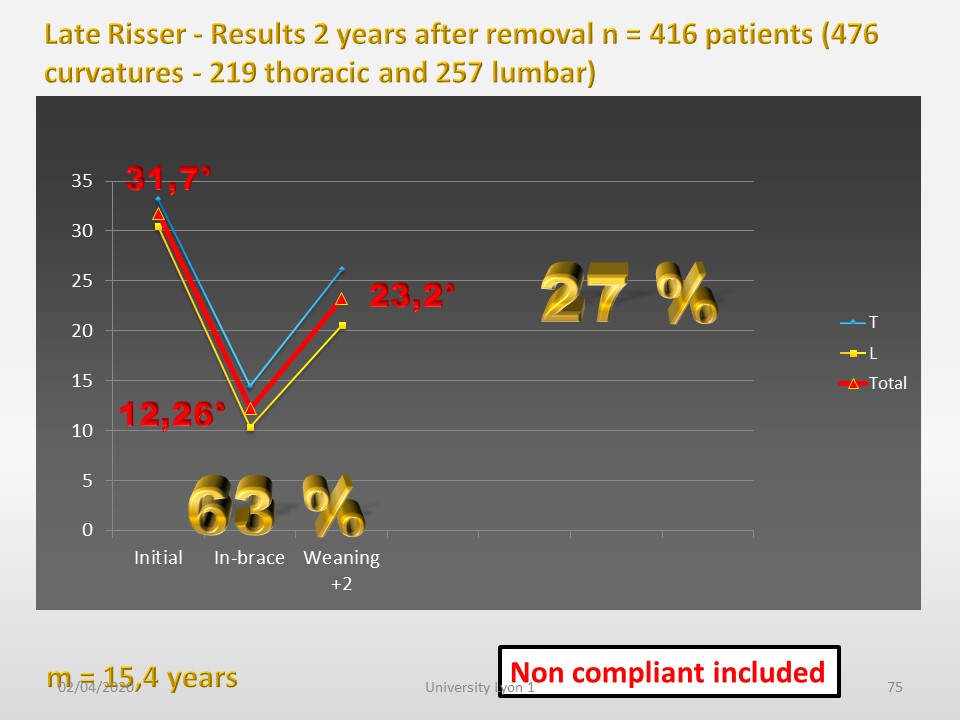
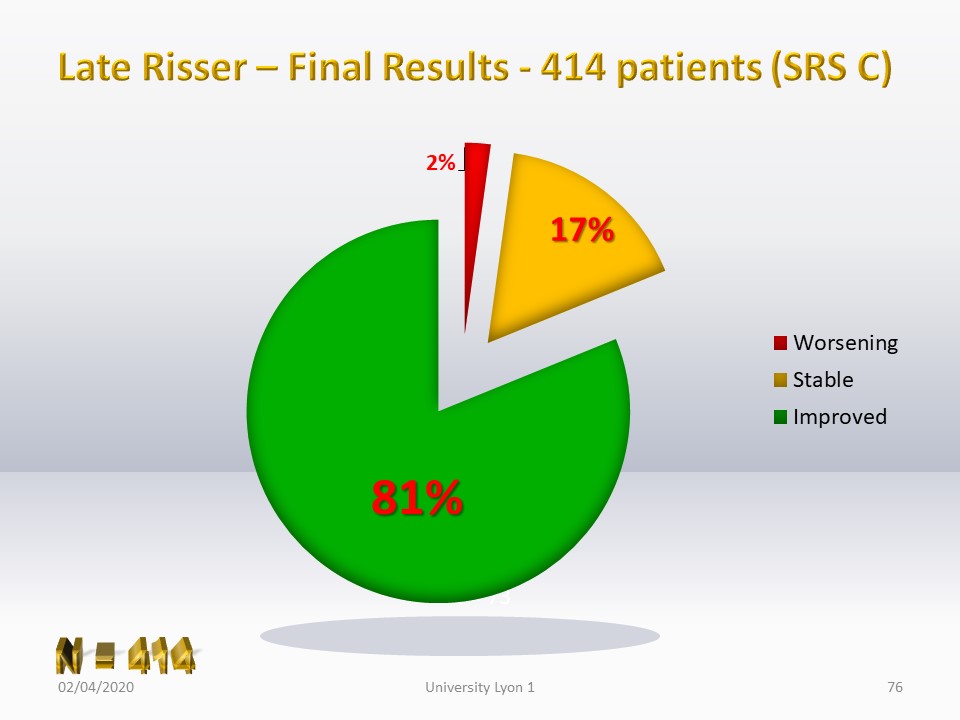
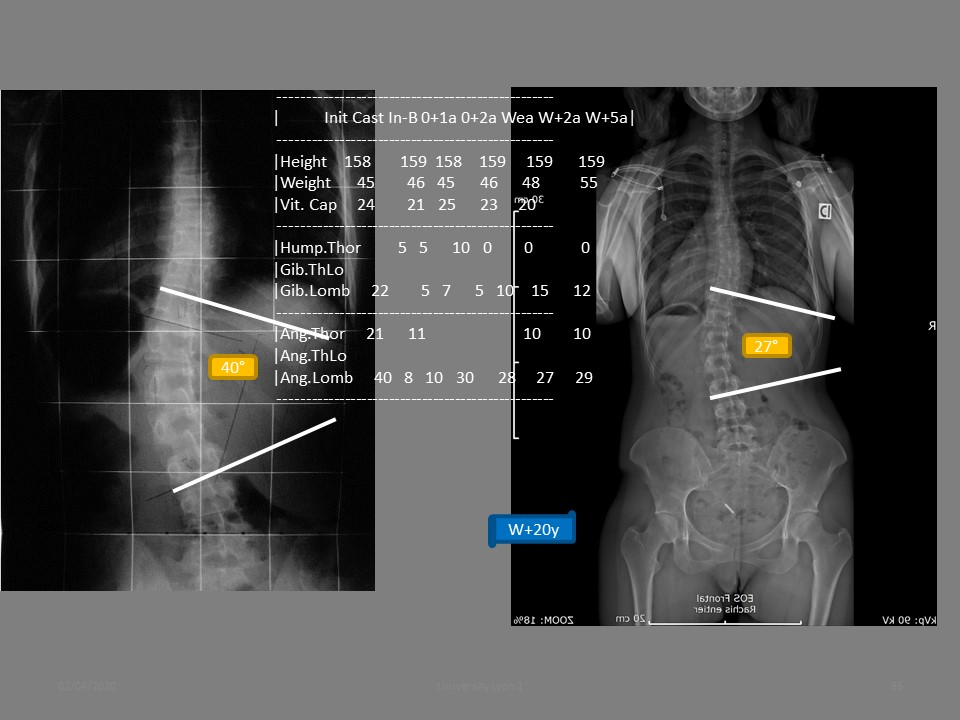
416 consecutive patients were reviewed 2 years after brace removal. average initial angulation of this group was 15 years and 5 months with an average angulation of 31,7°. It is therefore a group with relatively high angulation and at the end of growth. Very often, treatment is offered as an alternative to surgery. The average in-brace correction is 63% significantly lower than the general average due to the stiffness of the curves. The final correction of 27% corresponds to the action of the Lyon method on the soft tissues.
|
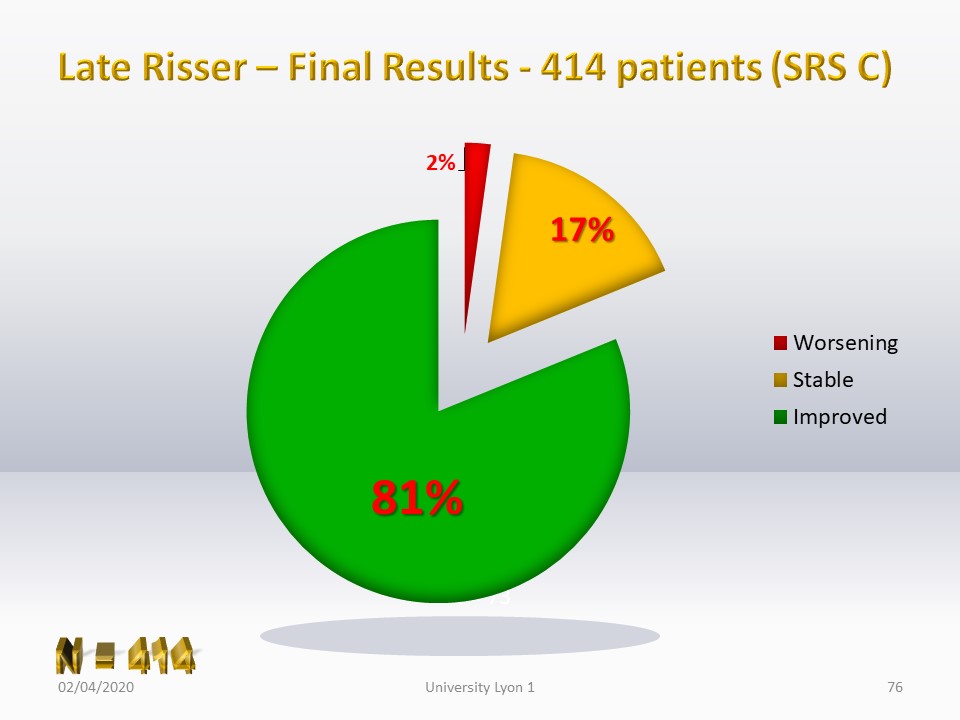 |
The final result is relatively constant given that non-compliant patients are included in the statistics.
|
 |
We found no correlations based on gender and initial angulation of scoliosis.
|
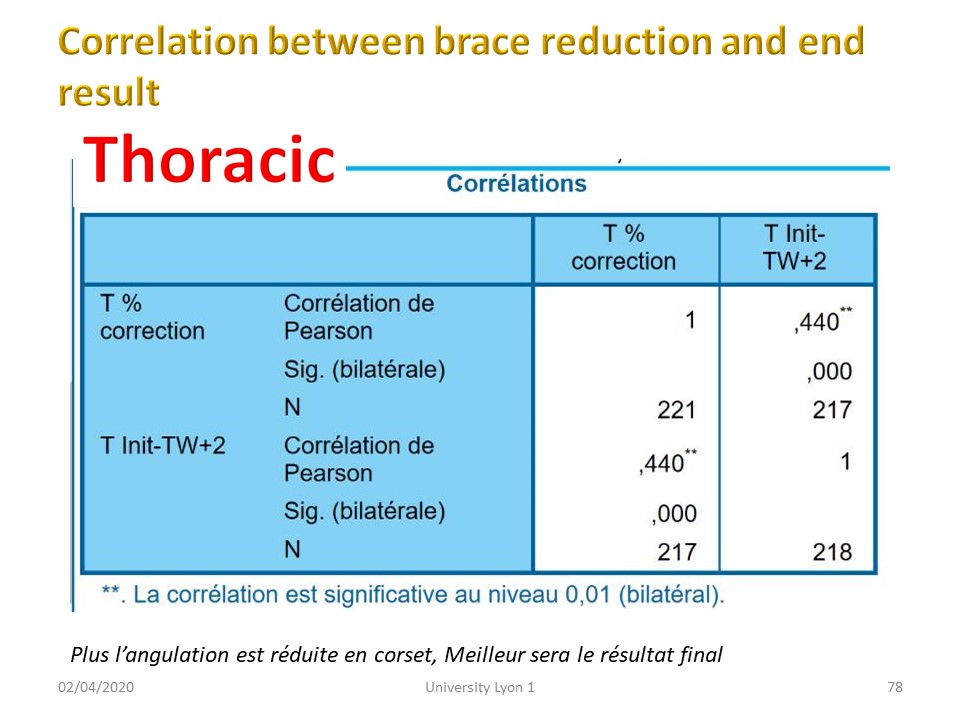 |
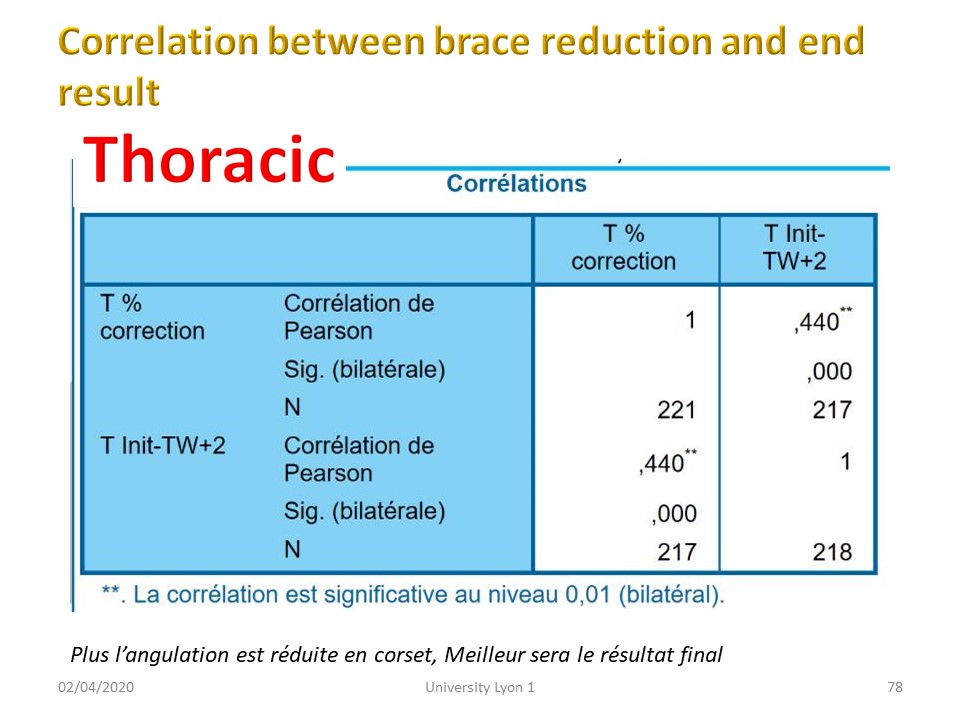
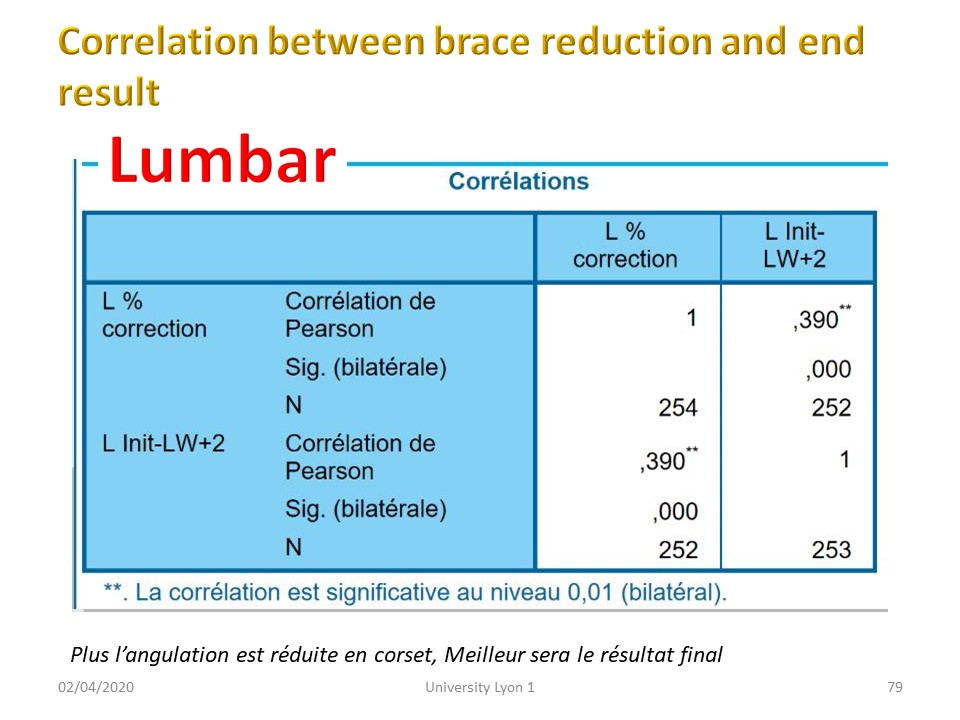
There is a significant correlation between the in-brace reduction and the final correction, but less significant than in the general statistic.
|
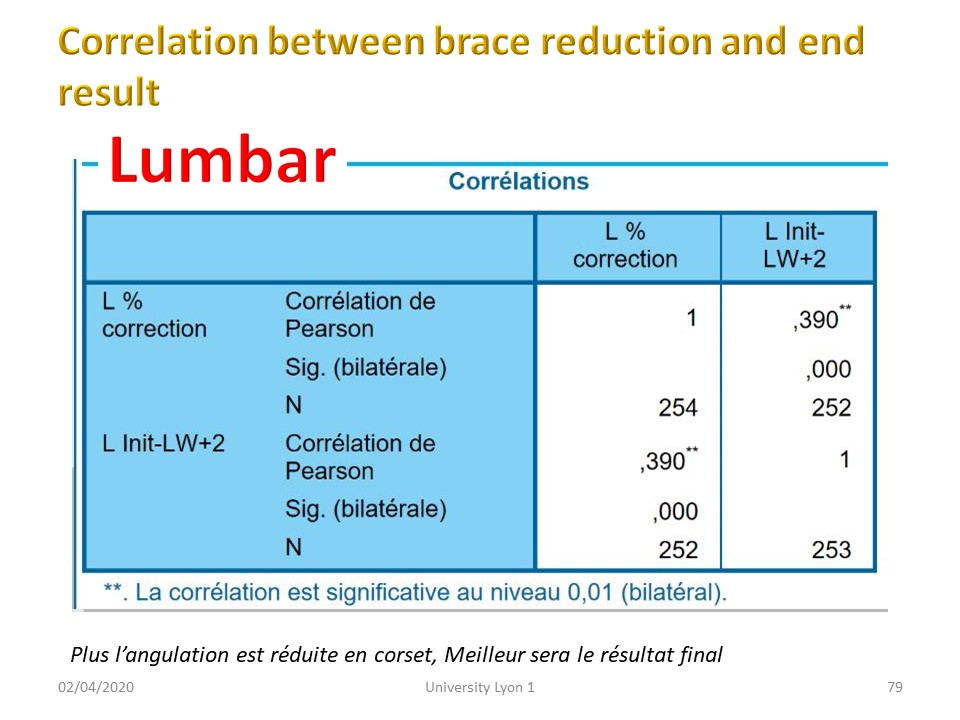 |
Both thoracic and lumbar.
|
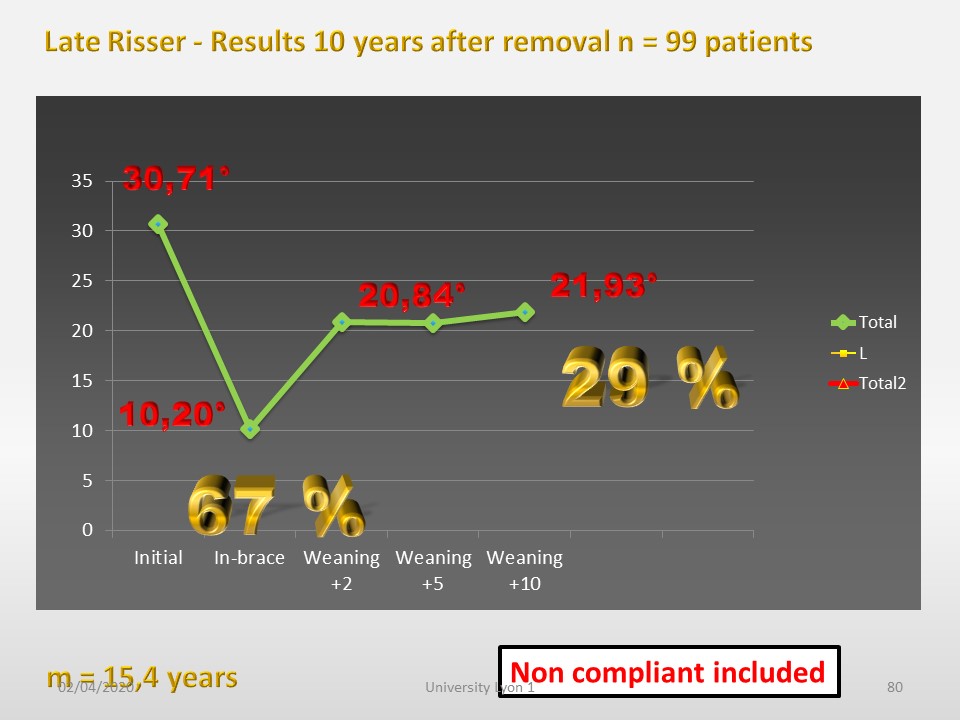 |
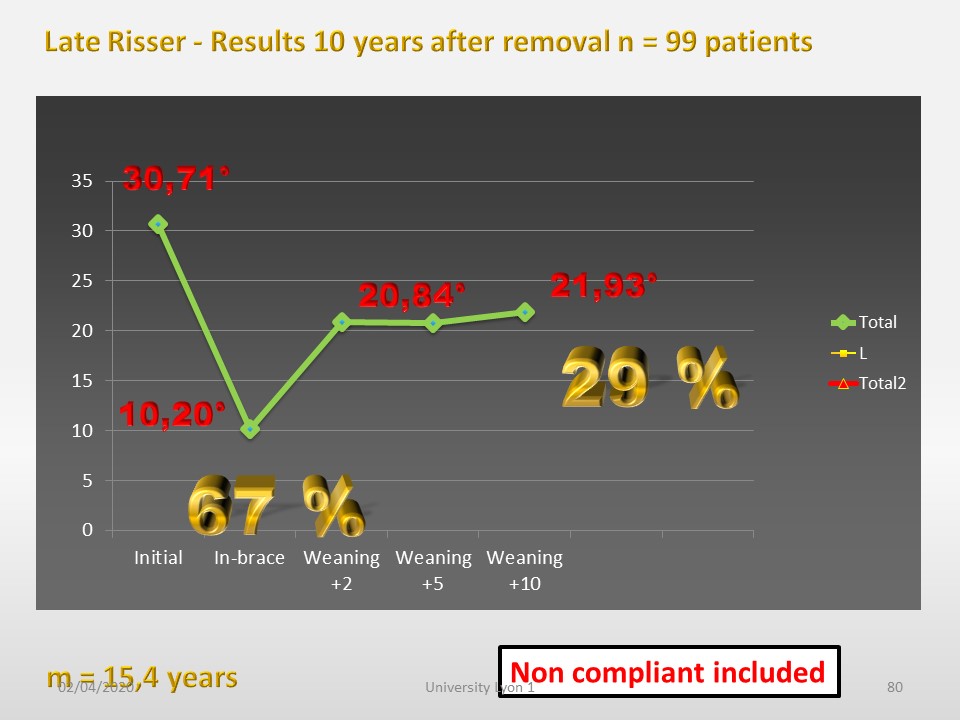
99 patients were seen 10 years after the brace was removed. The correction percentages are almost identical to those of the general statistic, but above all the stability over 10 years is very good and similar to what we found in the study of very long-term results.
|
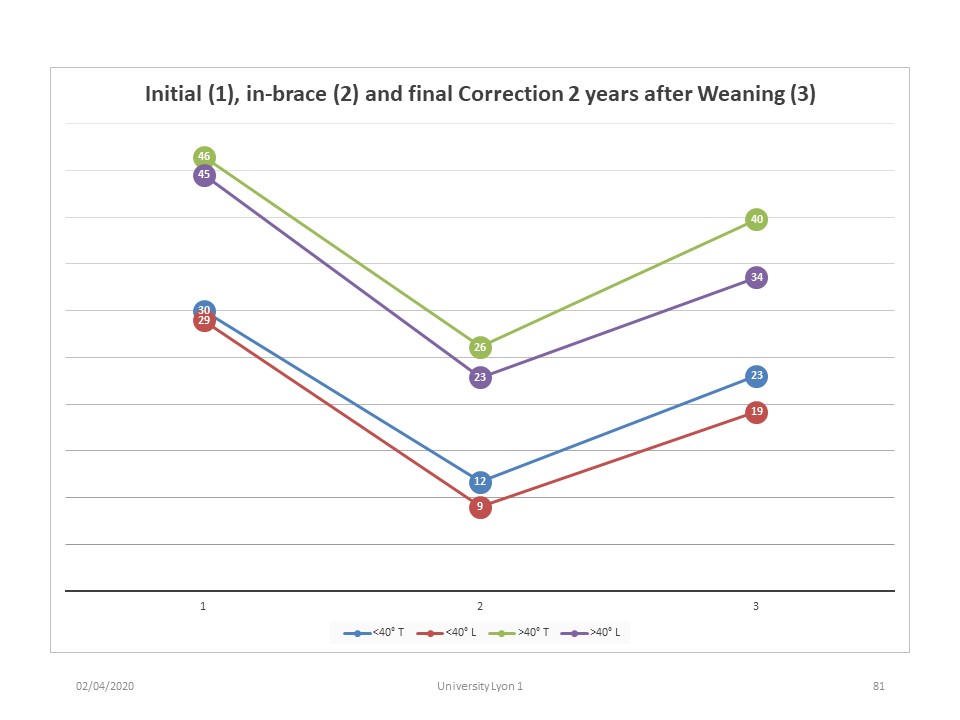 |
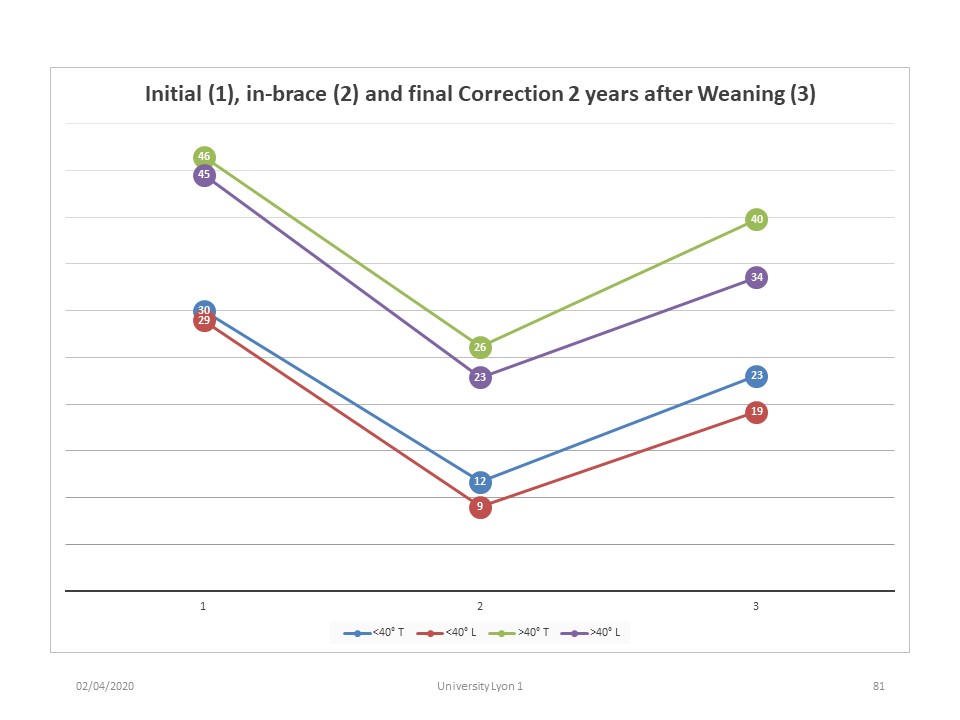
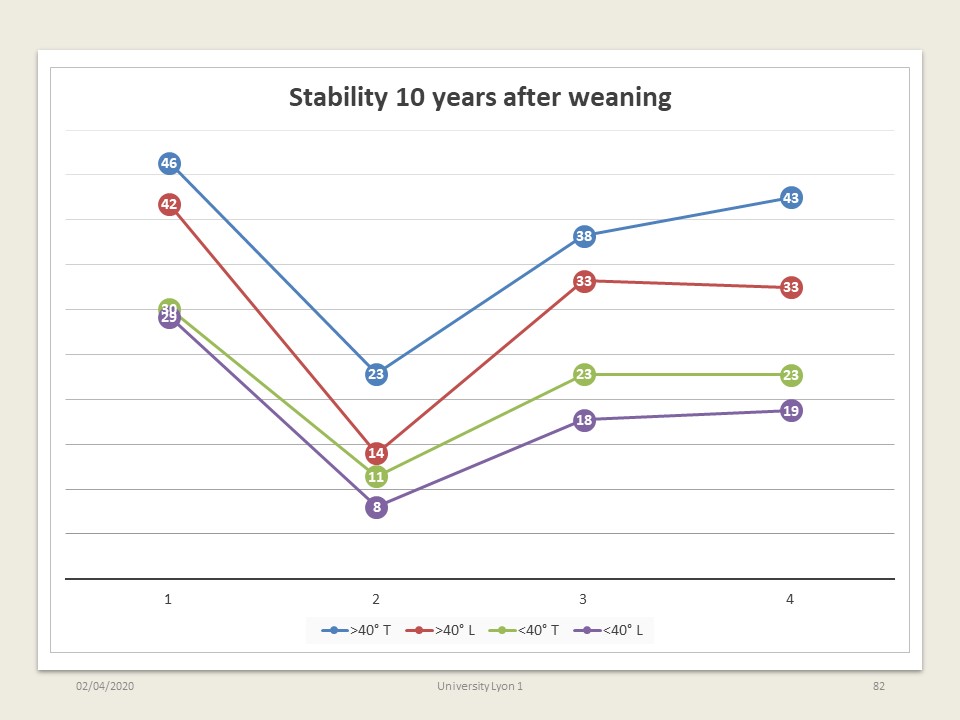
If we create 2 groups with angulation greater or less than 40°, we see an identical effectiveness of the treatment.
|
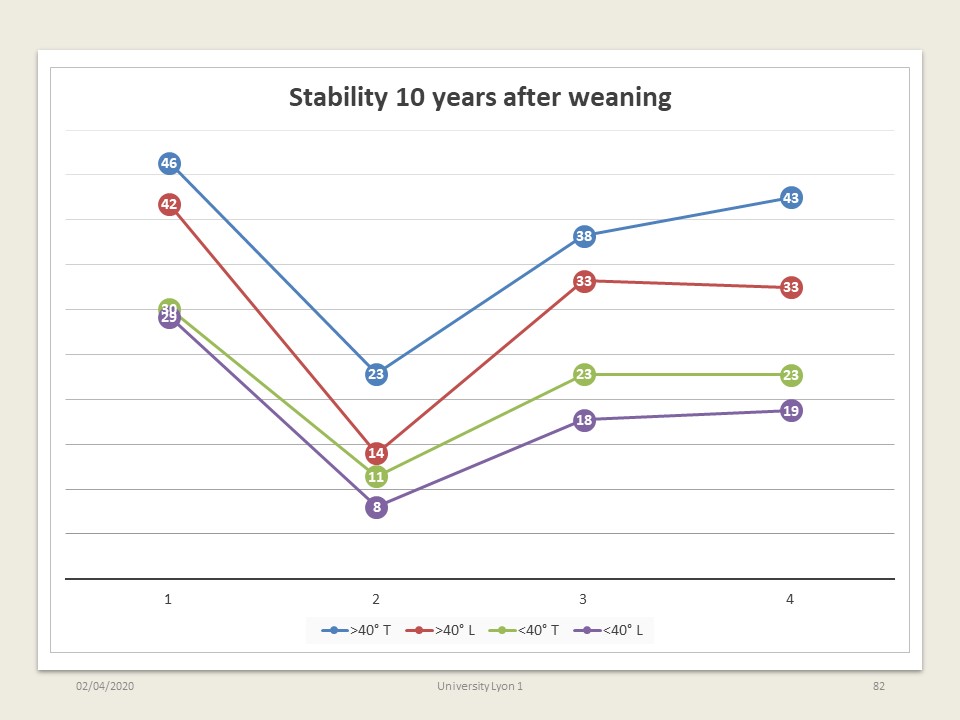 |
Similarly, for patients reviewed at 10 years of age, we do not see any difference for a cut-off of 40°.
|
 |
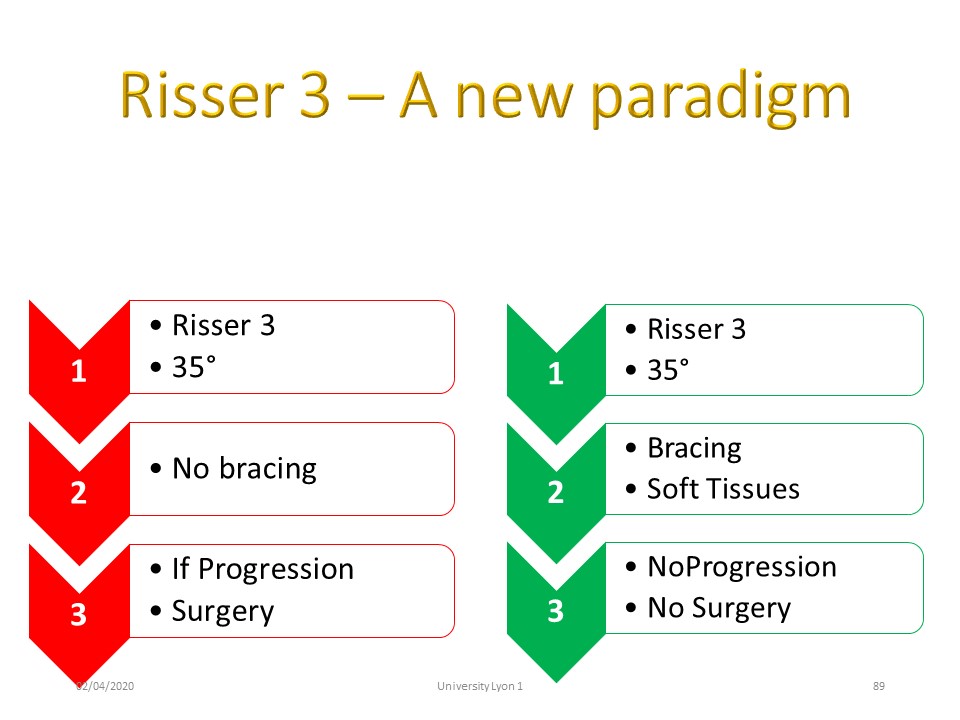
The end of bracing after Risser 3 results from the confusion between the criteria for assessing an orthopaedic treatment and the indications for this treatment. It is still possible to avoid surgery for a 40° curvature at Risser 3.
|
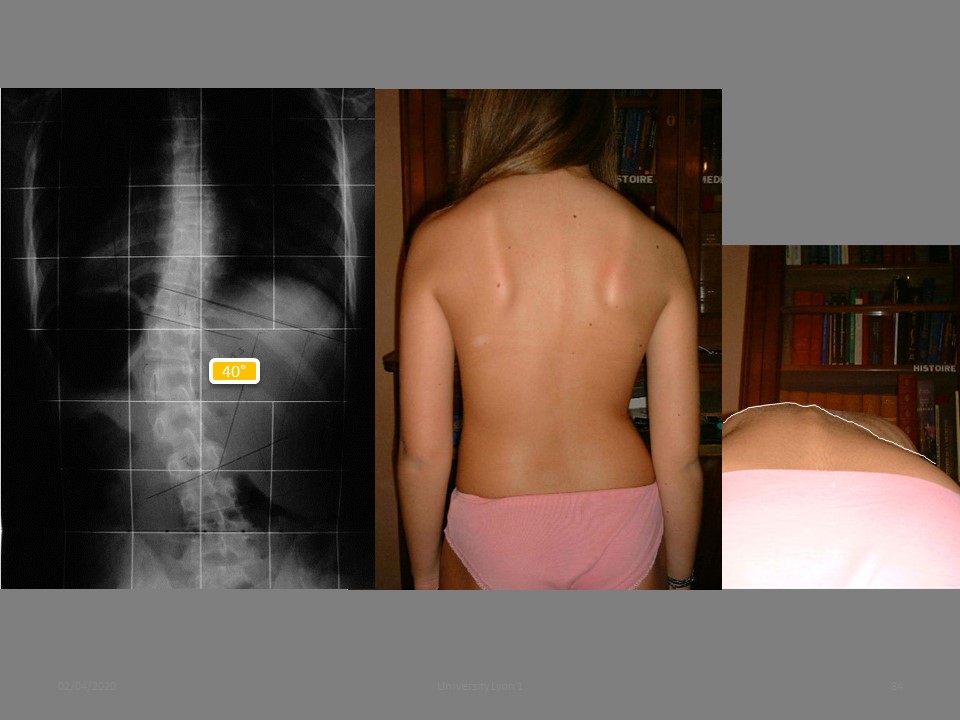 |
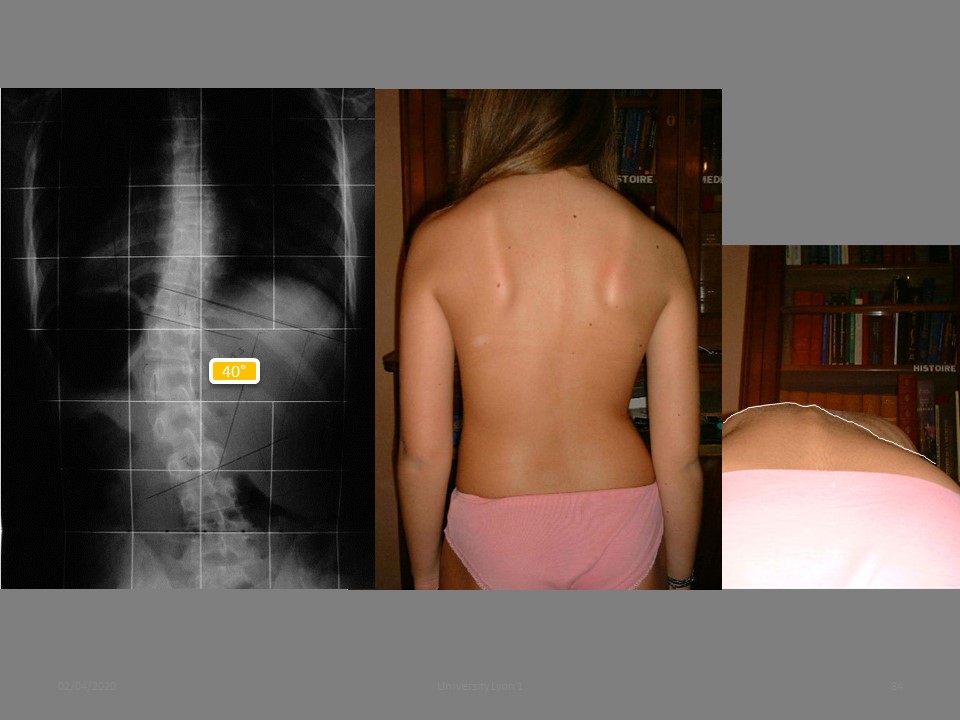
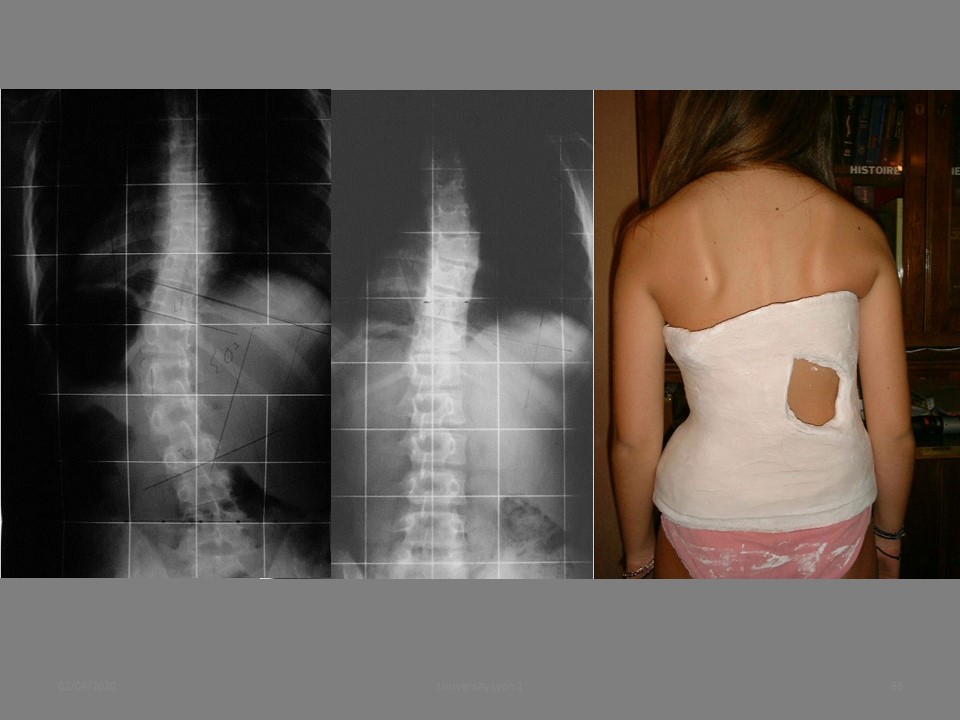
This child had a left thoracolumbar curvature of 40° at the end of height growth with discussion of surgery.
|
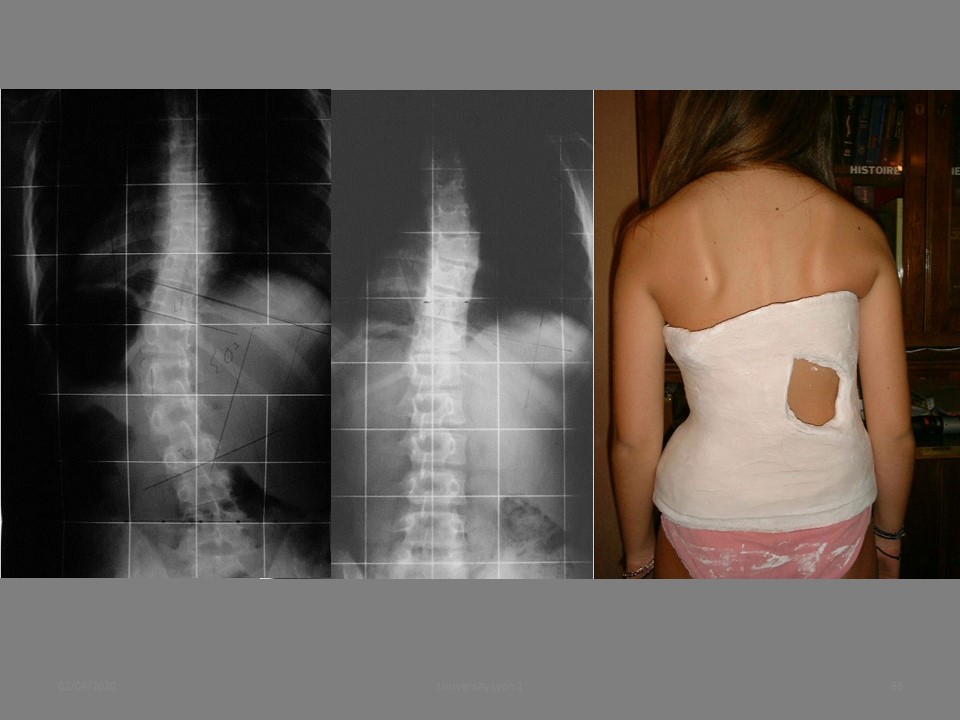 |
The plaster cast perfectly reduces curvature with remarkable untwisting.
|
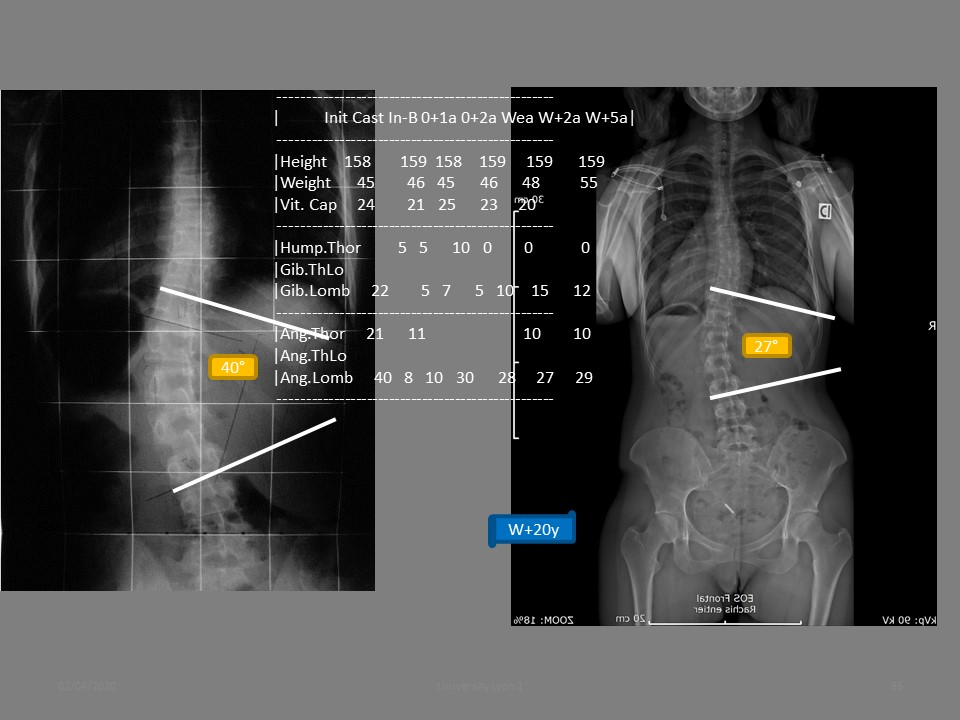 |
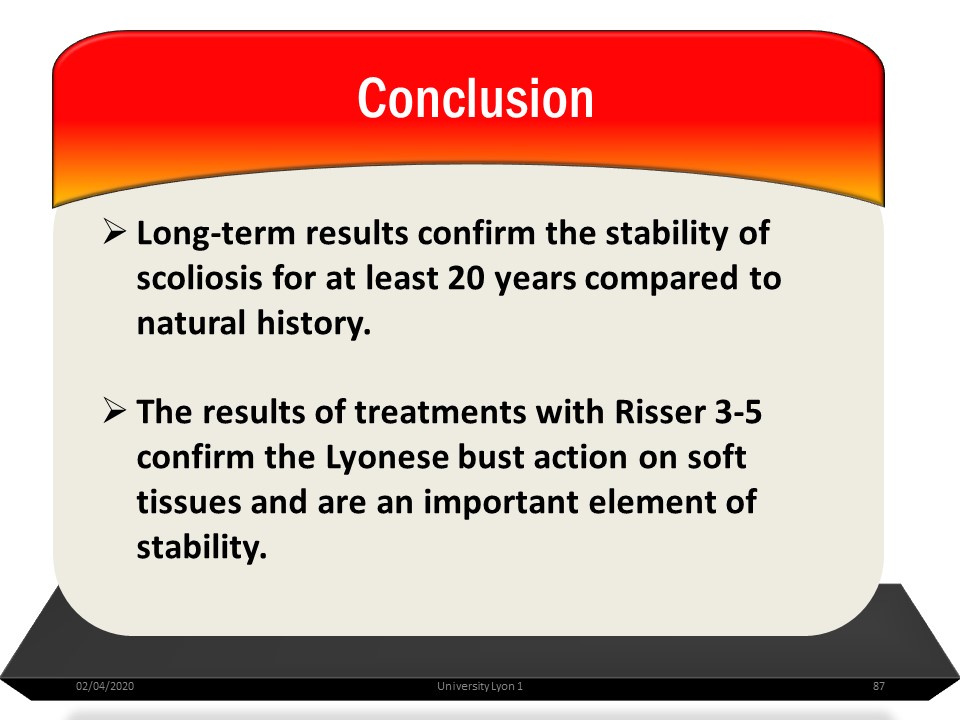
20 years after removal of the corset, the angulation is 27°, perfectly stable without the need for surgery.
|
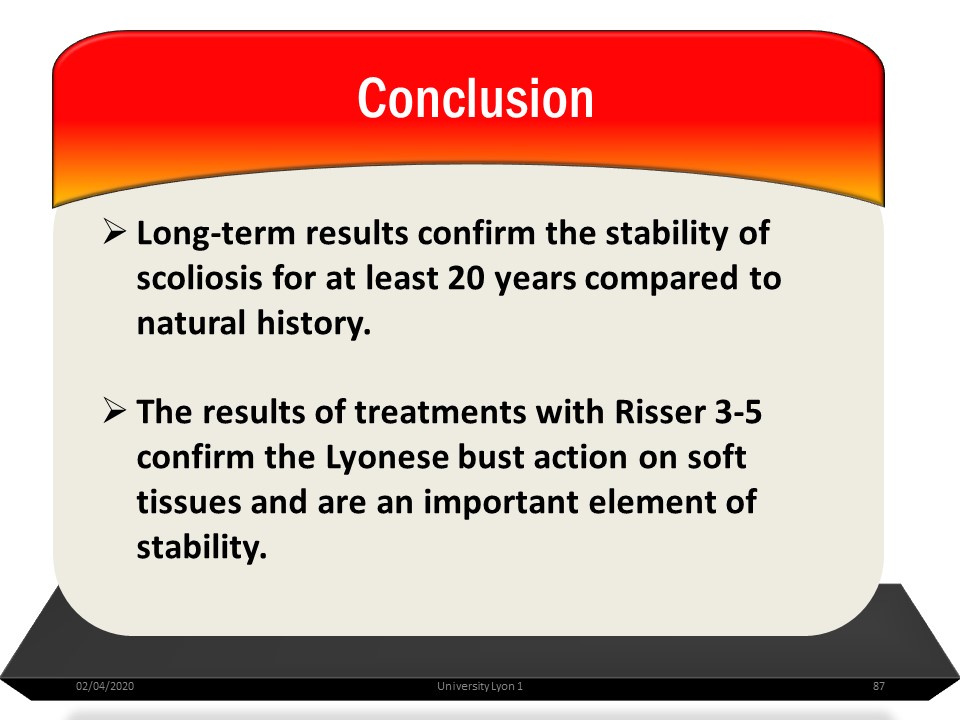 |
The results of treatments with Risser 3-5 confirm the Lyon brace action on soft tissues and are an important element of stability.
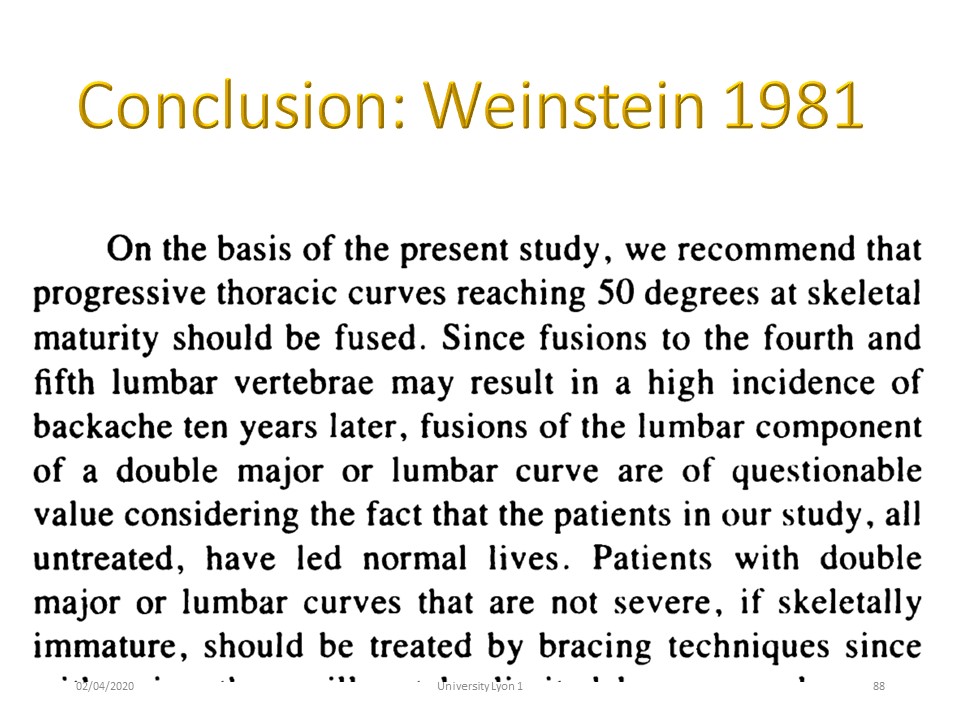
|
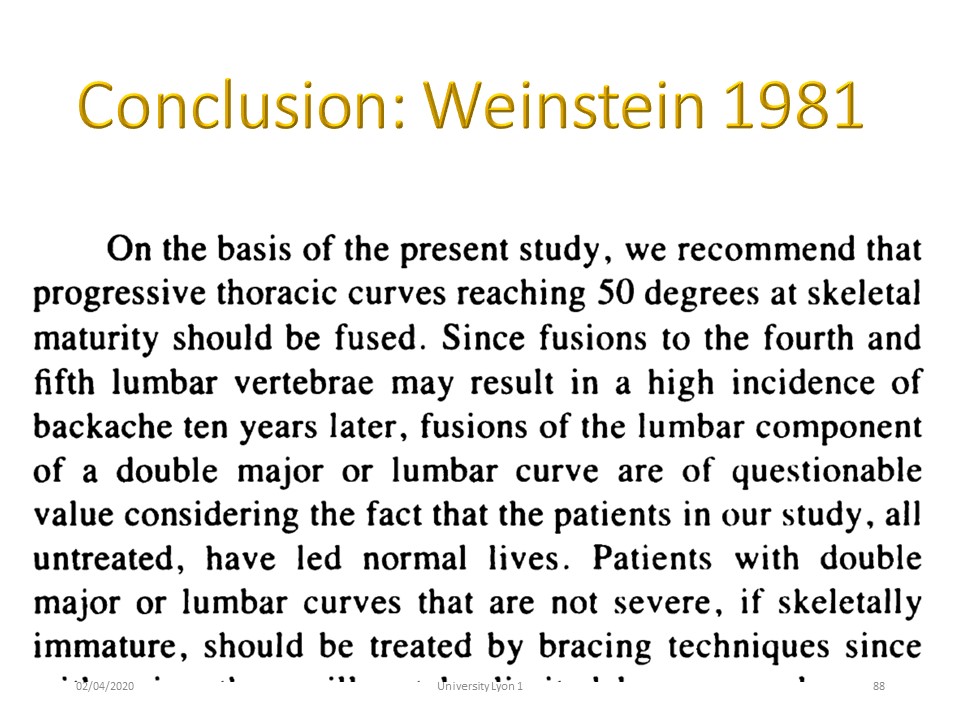 |
This conclusion is consistent with Weinstein's conclusion in 1981 which set the surgical limit at 50° for thoracic curvatures.
|
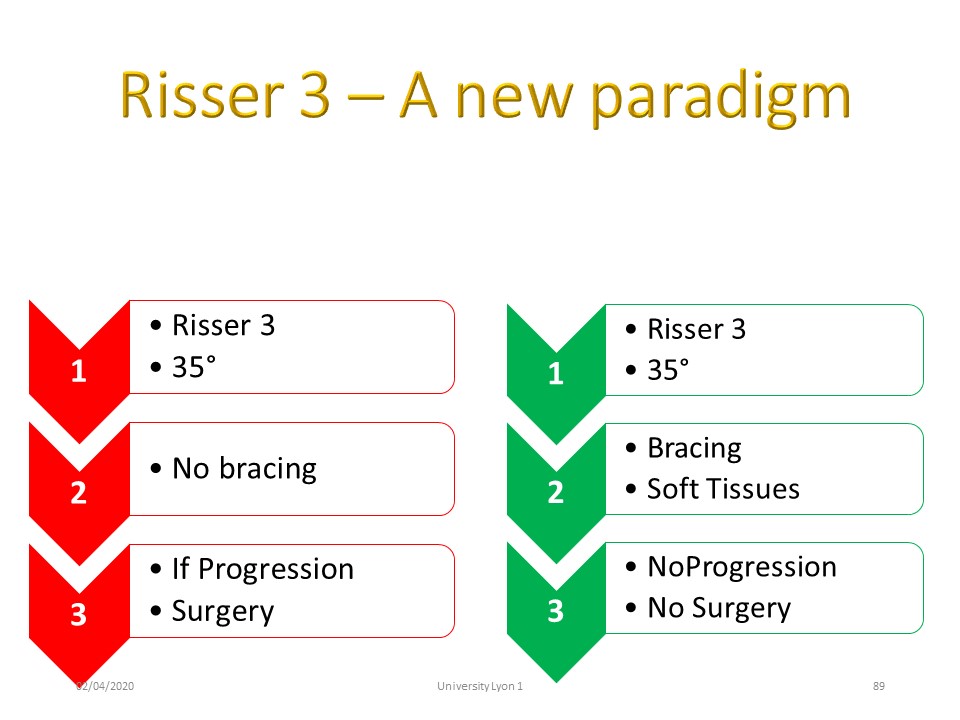 |
With the realization of a hypercorrective brace effective on soft tissues (it is no longer a question of guiding growth), and a precise protocol, it is possible to stabilize scoliosis without surgery.
|
 |
|
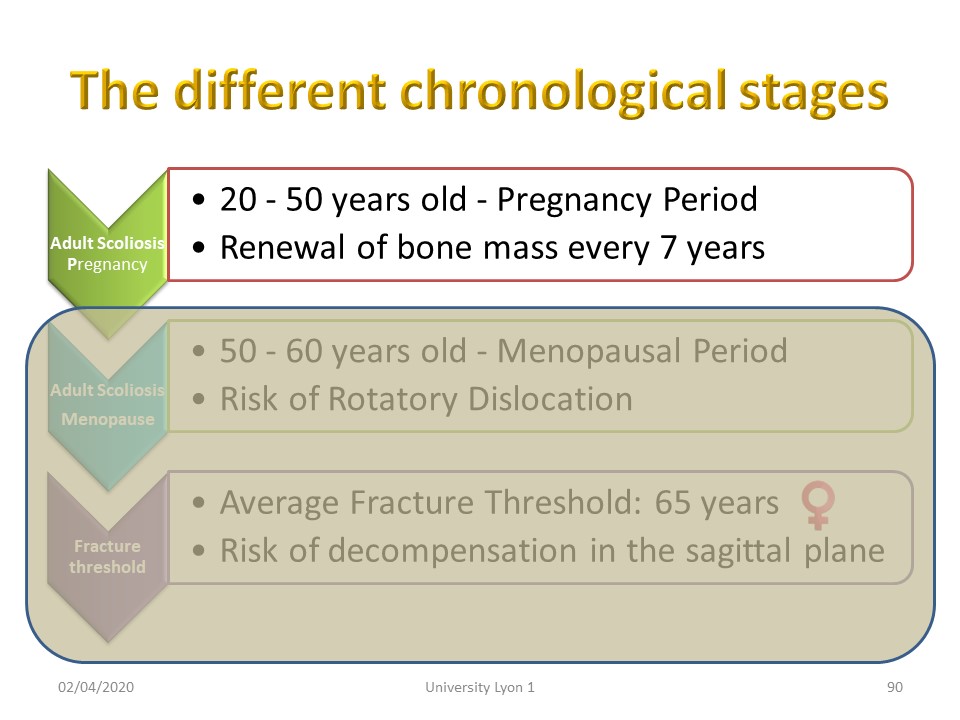 |
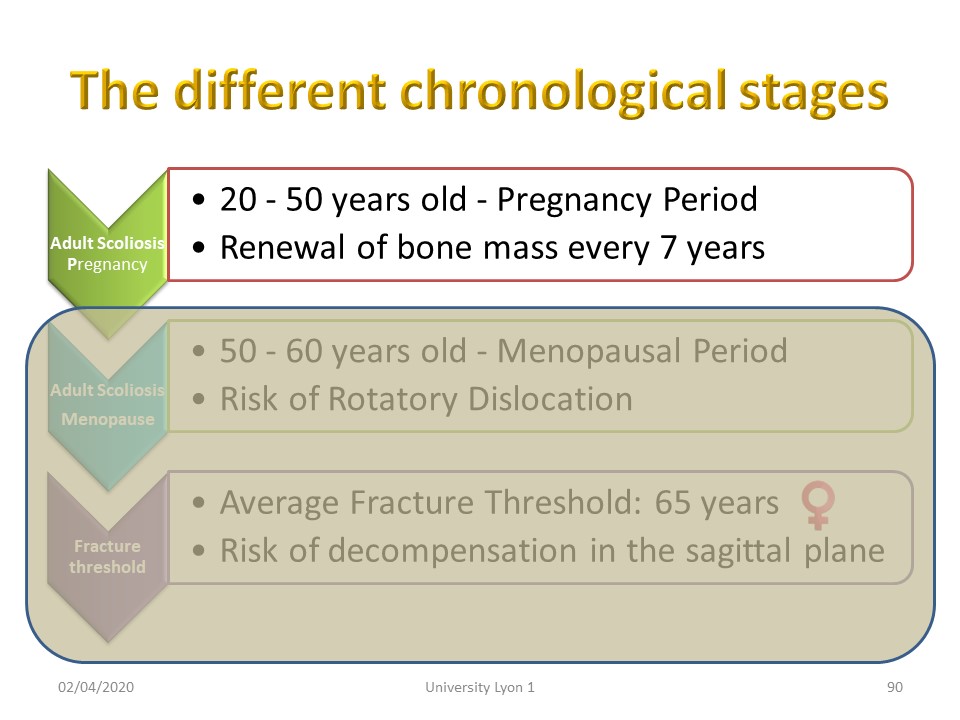
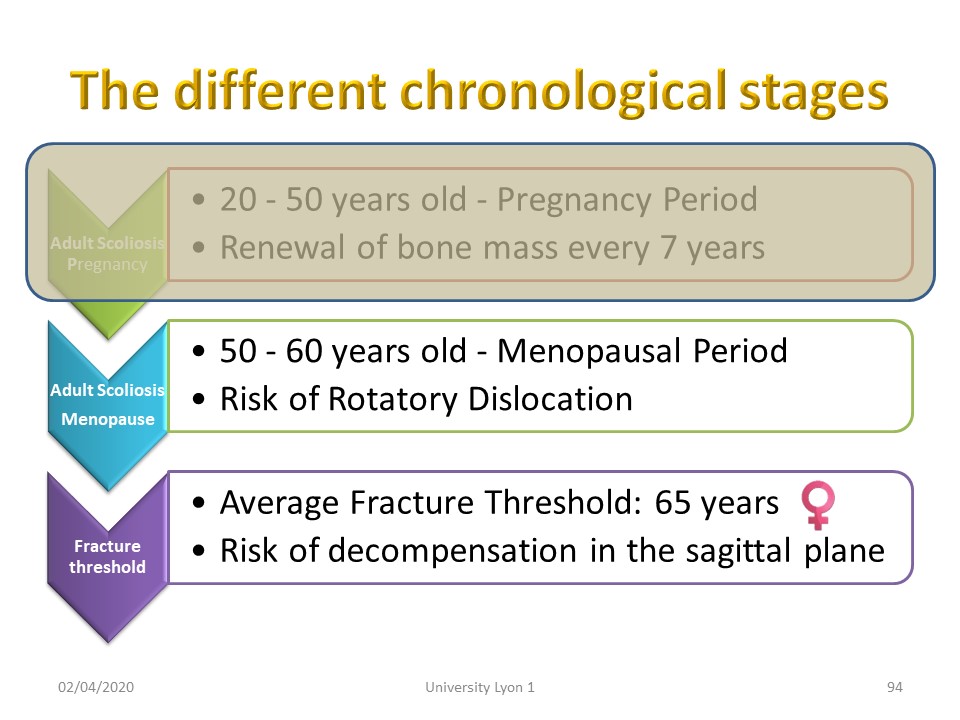
In adulthood bone mass is renewed every 7 years and scoliosis can continue to evolve by 0.5 ° / year between 30 and 40 ° and more than 1 ° per year beyond 40 °.
|
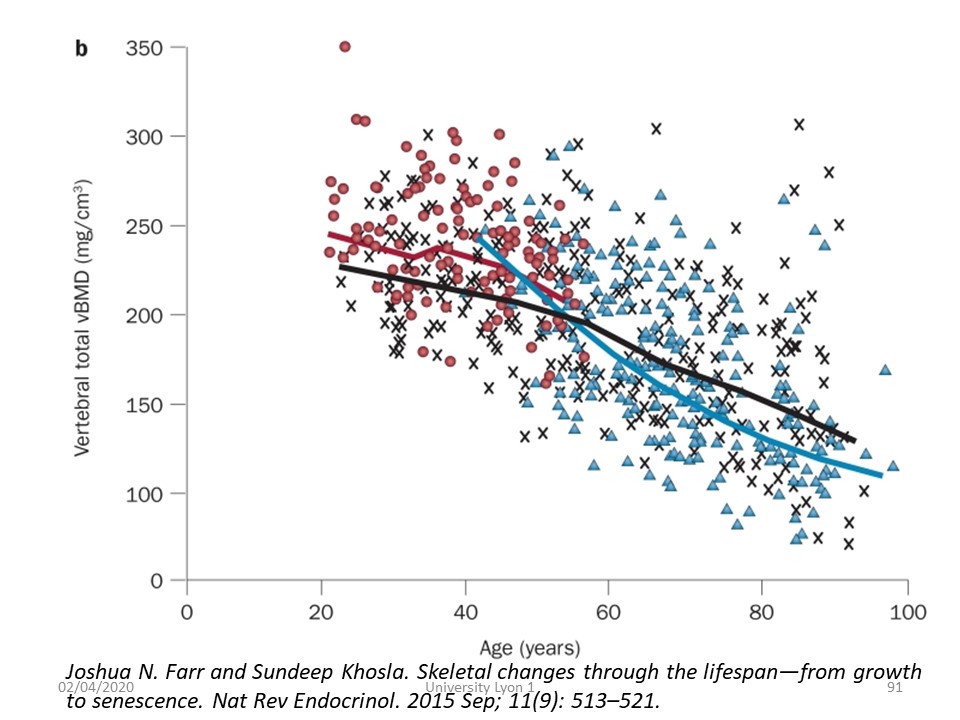 |
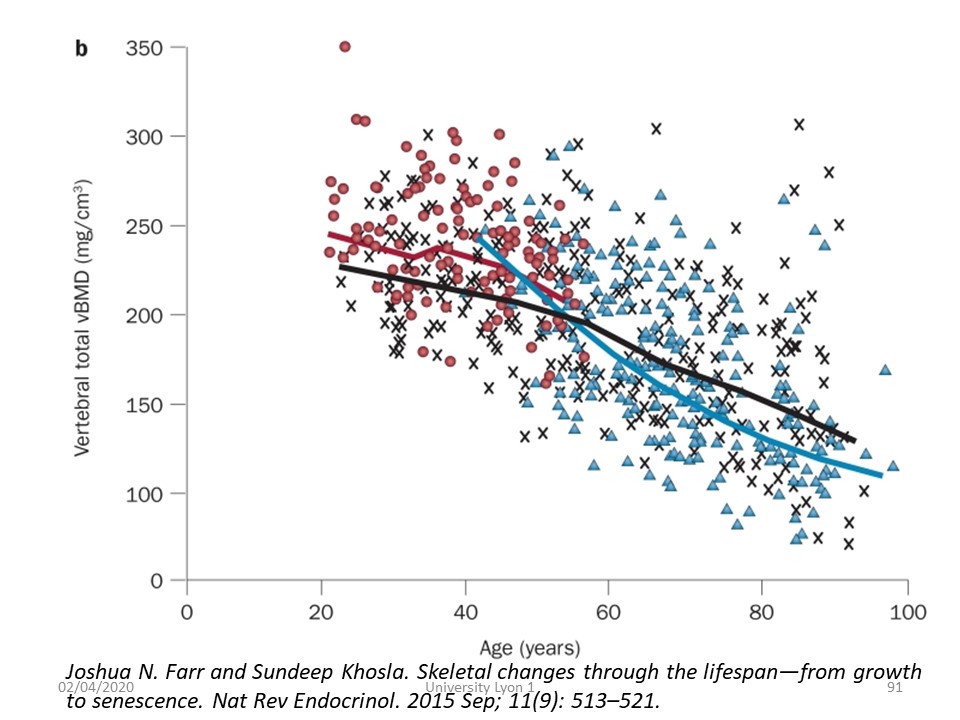
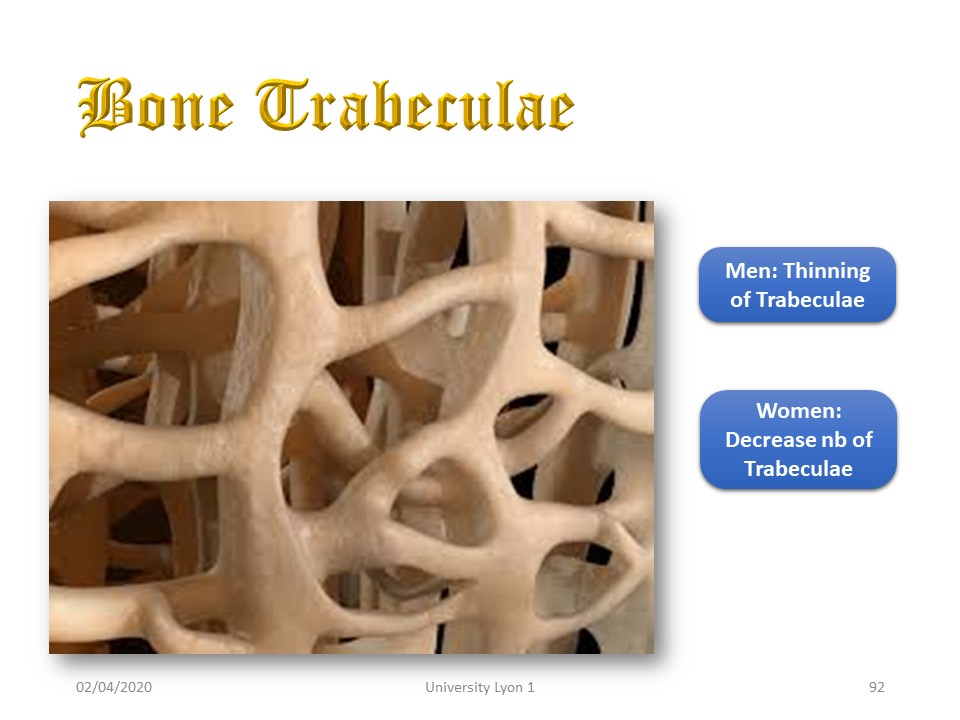
Trabecular bone loss tends to increase during the menopausal period to reach the fracture threshold at age 65 in women.
|
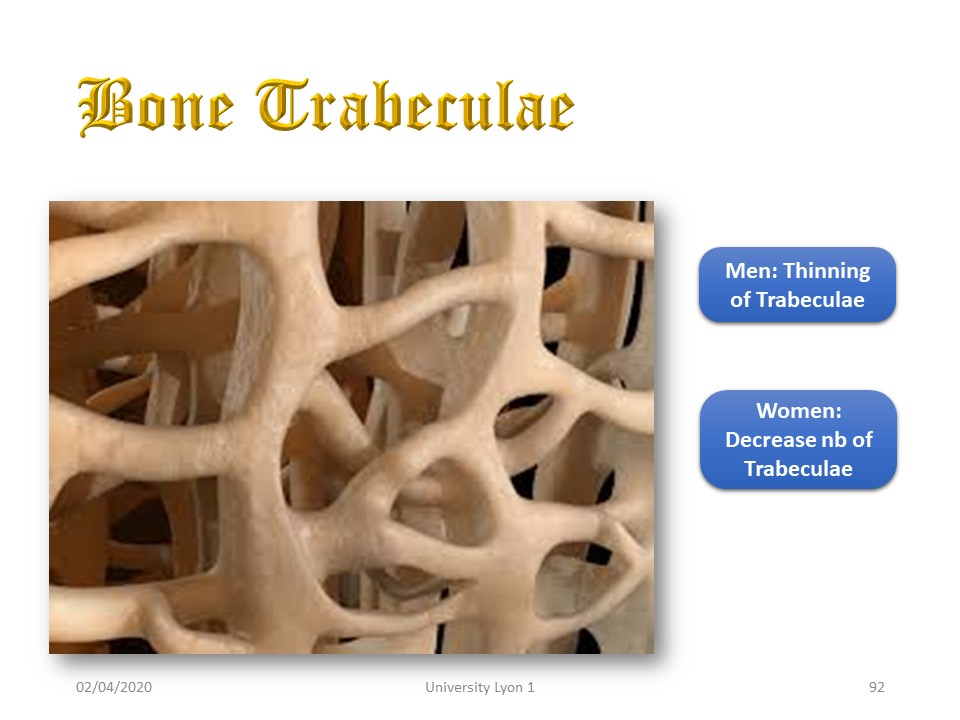 |
In men, trabeculae do not diminish but become thinner. The fracture threshold in men is 85 years old.
|
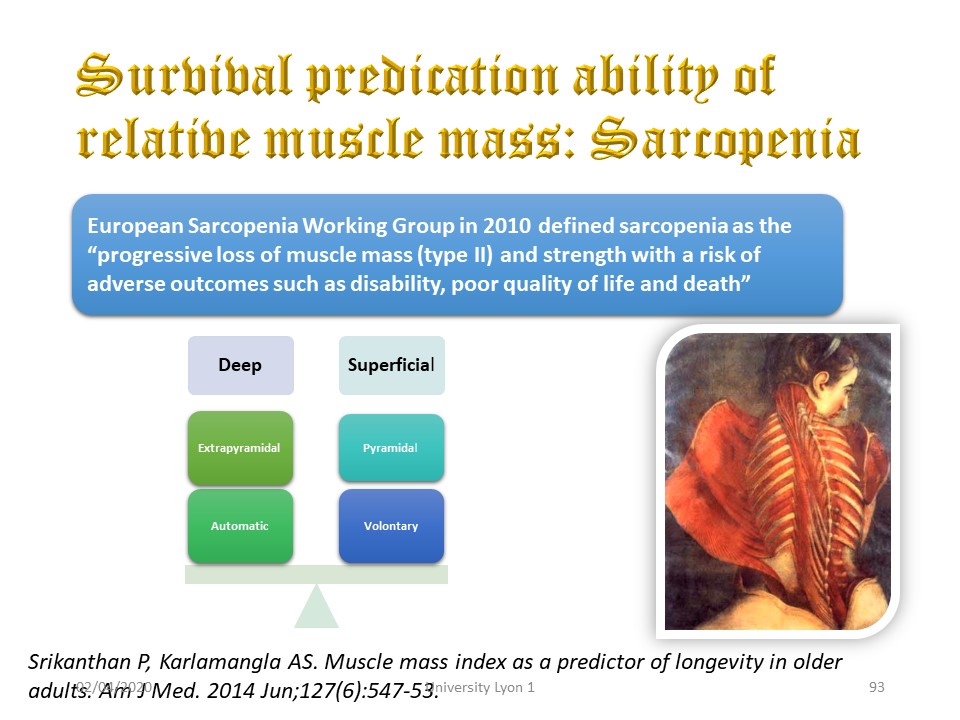 |
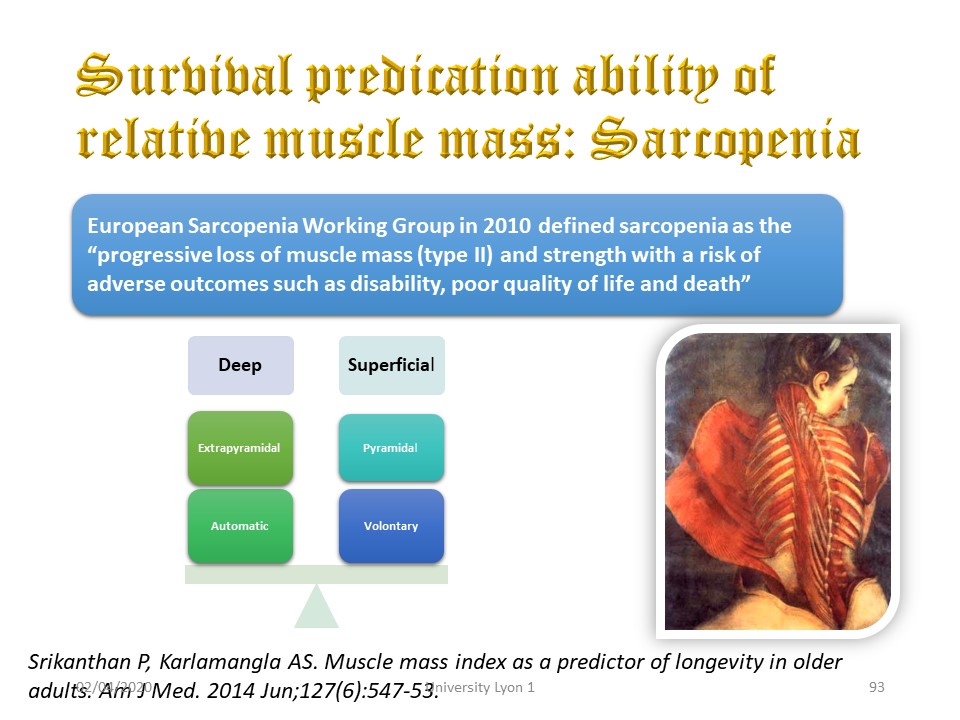
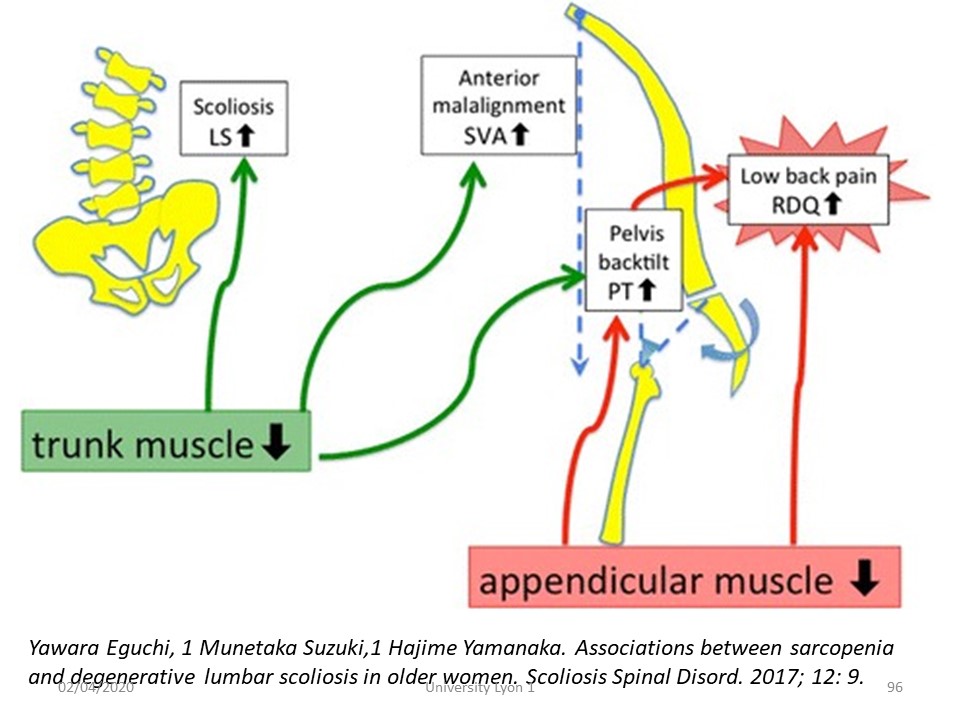
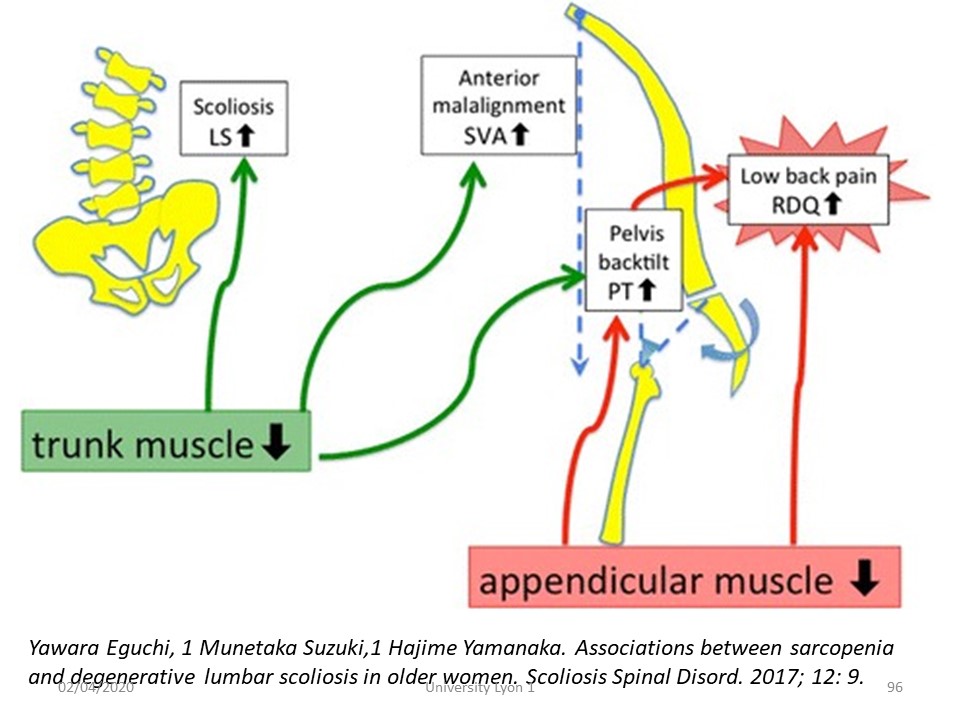
Osteopenia is accompanied by a sarcopenia that atrophies the pyramidal voluntary muscle mass but does not affect the extra-pyramidal muscle mass.
|
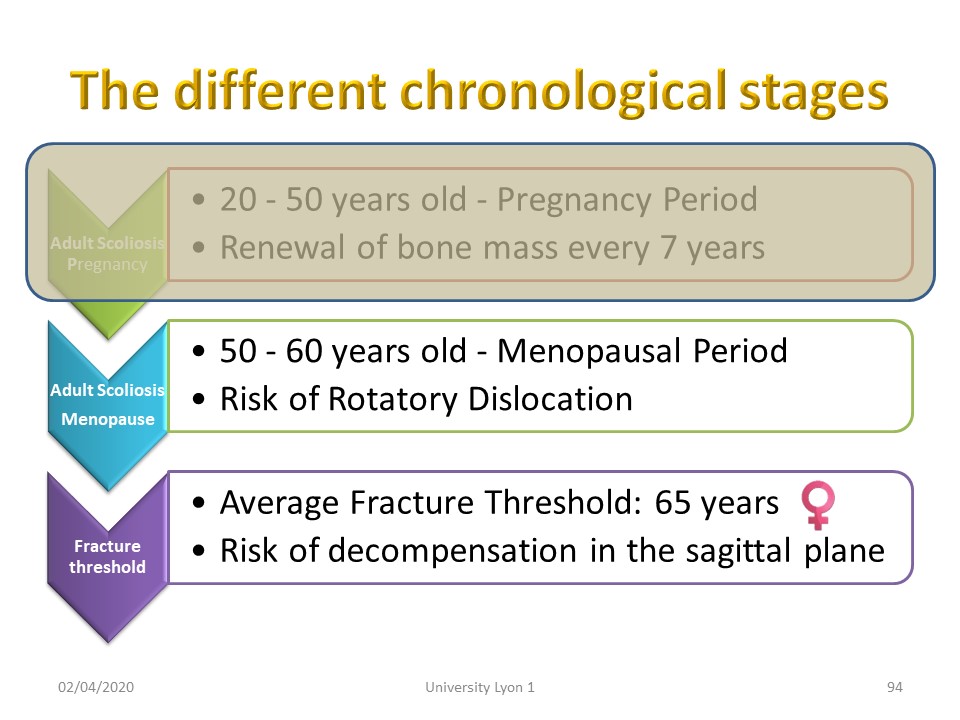 |
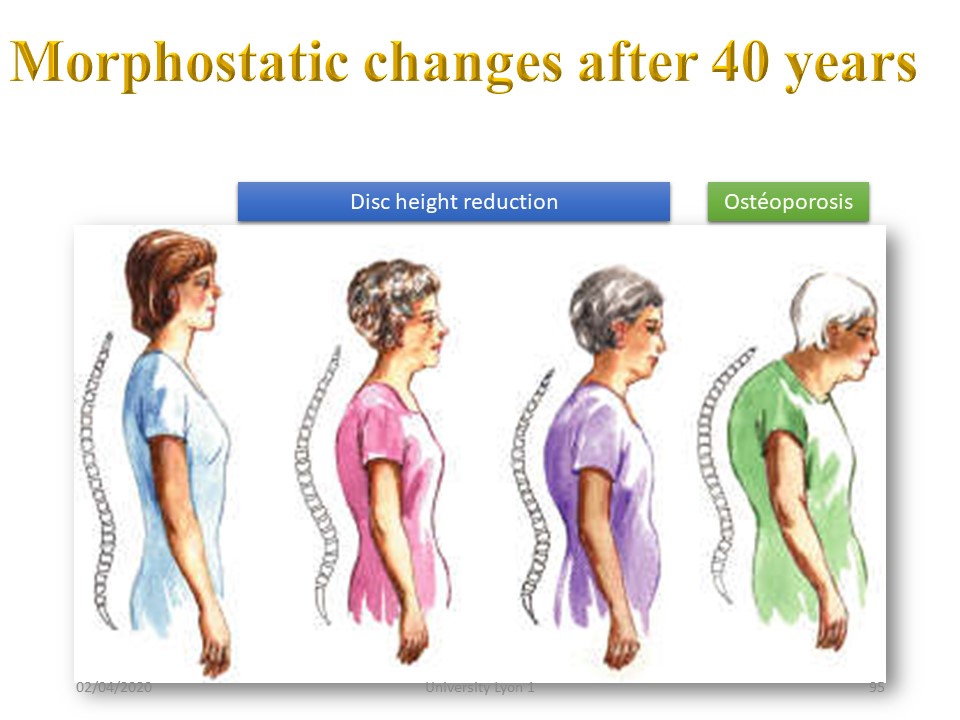
In the menopausal period osteopenia and sarcopenia is associated with discopathy and decrease of height of the intervertebral discs.
|
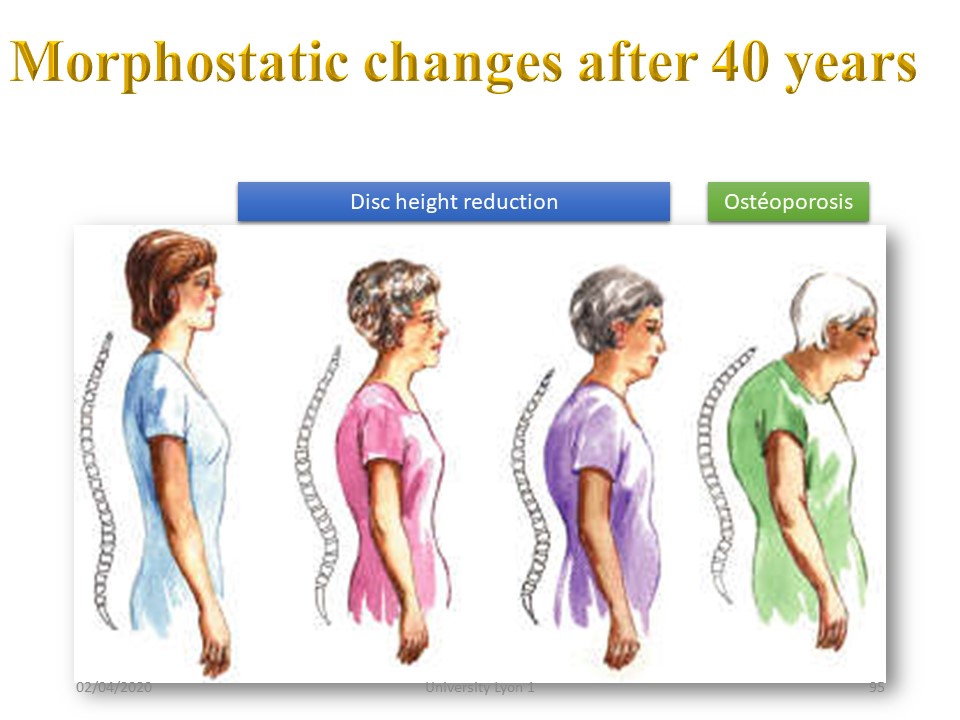 |
Morphostatic varies with age. The two main phenomena are: 1, The decrease in height of the discs causing hypo lordosis and hyperkyphosis of compensation. 2. Osteoporosis which most often causes high thoracic kyphosis with progressive micro-vertebral compression,
|
 |
Abdominal hypotonia promotes pelvic retroversion and constitutes a vicious circle with hypolordosis related to disc height decrease and osteoporotic thoracic kyphosis.
|
| > |
Comment in the certification part of the website
To view the full video presentation register for the certification course” www.scoliosisandspineonlinelearning.com
|
 |
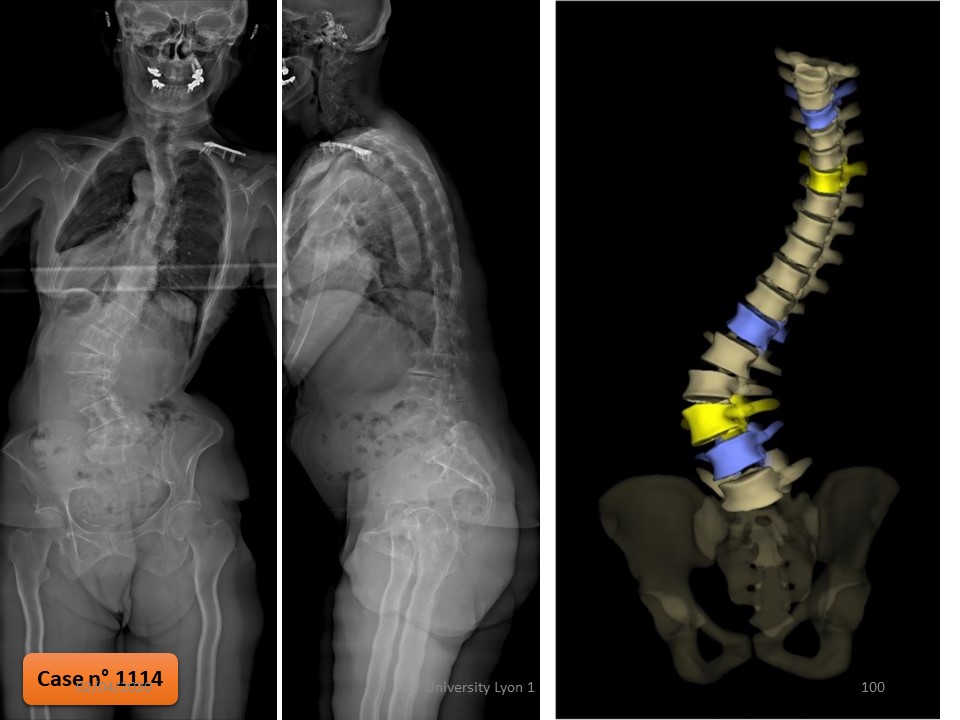
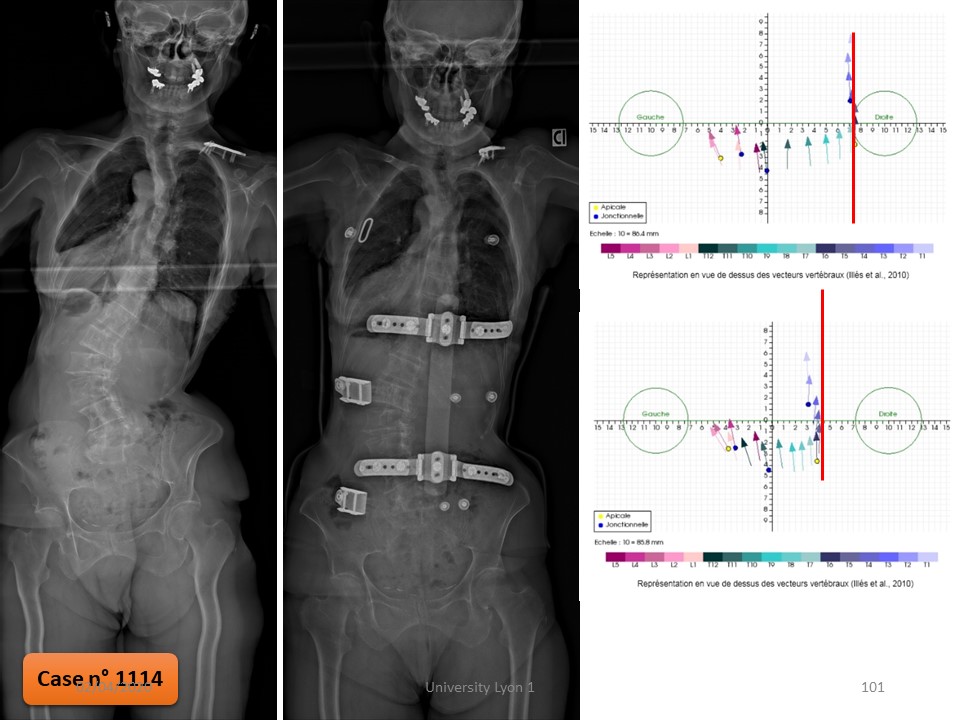
This 67-year-old patient has a very strong imbalance of the occipital axis of 40 cm to the right. The scoliosis T12-L4 is 65 °. A first polyethylene brace redone 3 times in another hospital, was not supported. A walker has been prescribed. In brace, the correction of the imbalance of the occipital axis is significant.
|
 |
Similarly, in the sagittal plane, while the patient has difficulties to stand alone, orthosis is much more balanced.
|
 |
Initially scoliosis Cobb angle is 65 °. The reducibility test is favorable, and the patient corrects herself when she is lifted under the arms.
|
 |
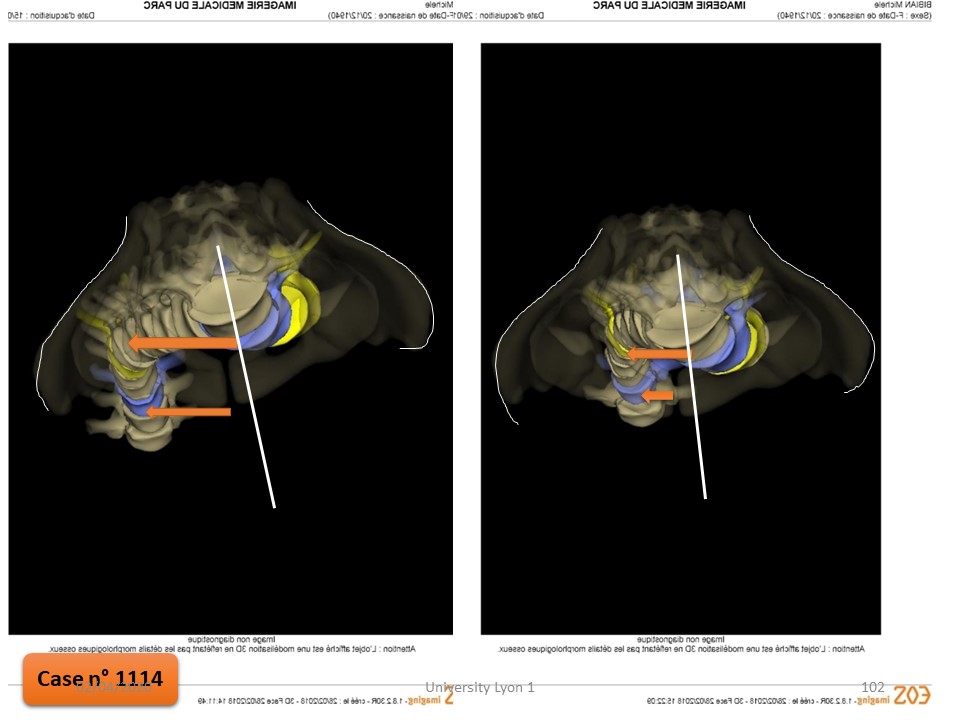
Indeed, the in-brace angulation is reduced to 25 ° with under EOS 3D a refocusing along the vertical axis.
|
 |
The recentering at the lumbar level is linked to the translation with a horizontal iliac plate that pushes as a caterpillar the lumbar vertebrae on the median line. Only polycarbonate allows a bending brake of 120 °.
|
 |
The improvement is also clearly visible in the sagittal plane.
|
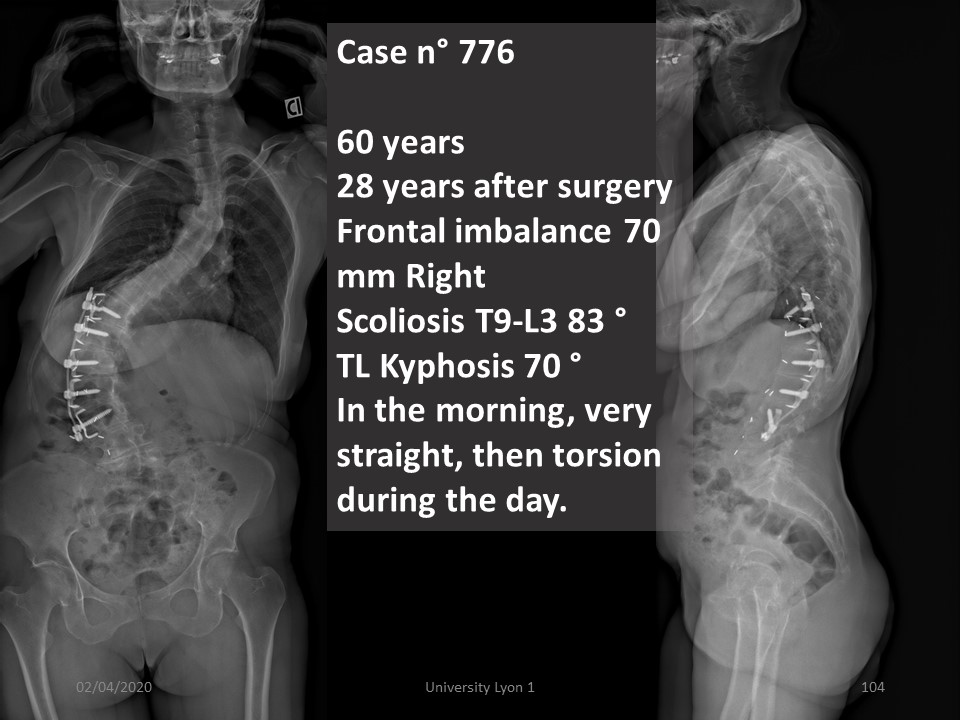 |
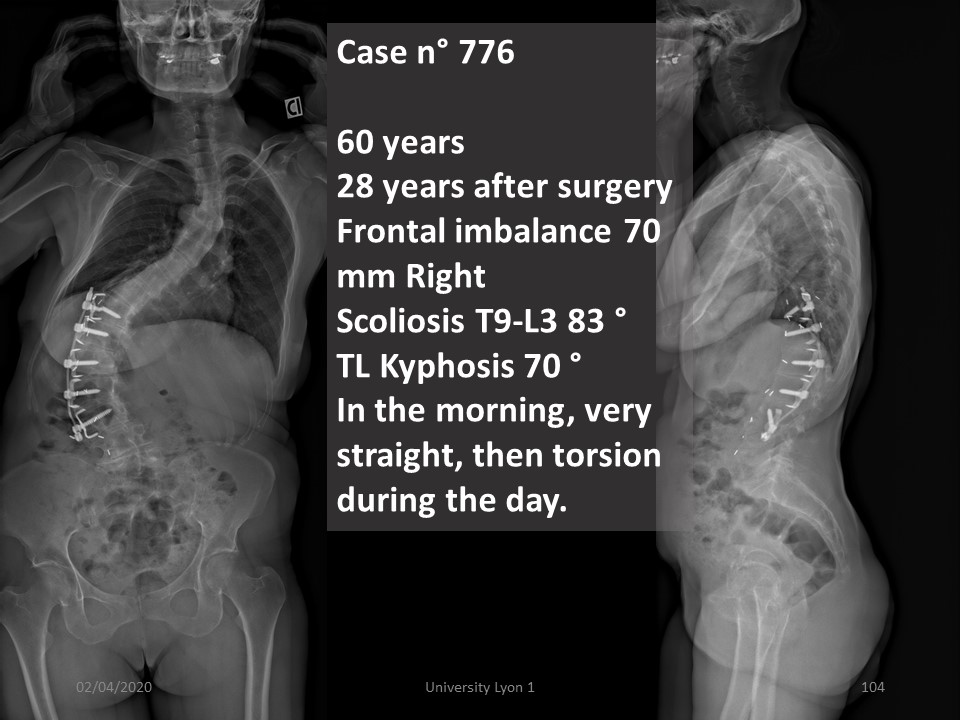
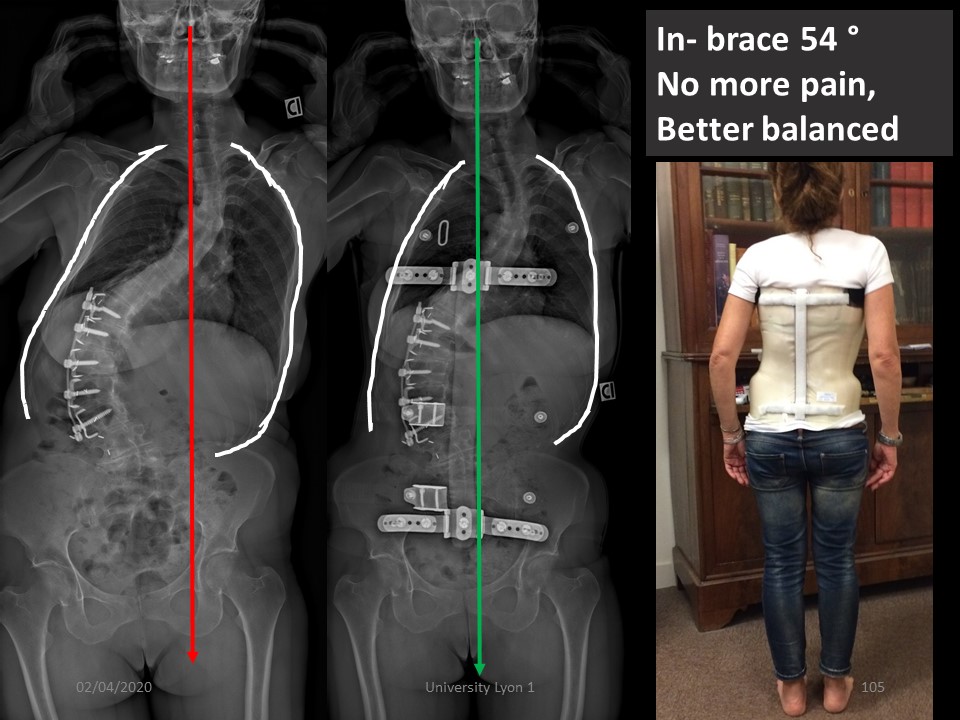
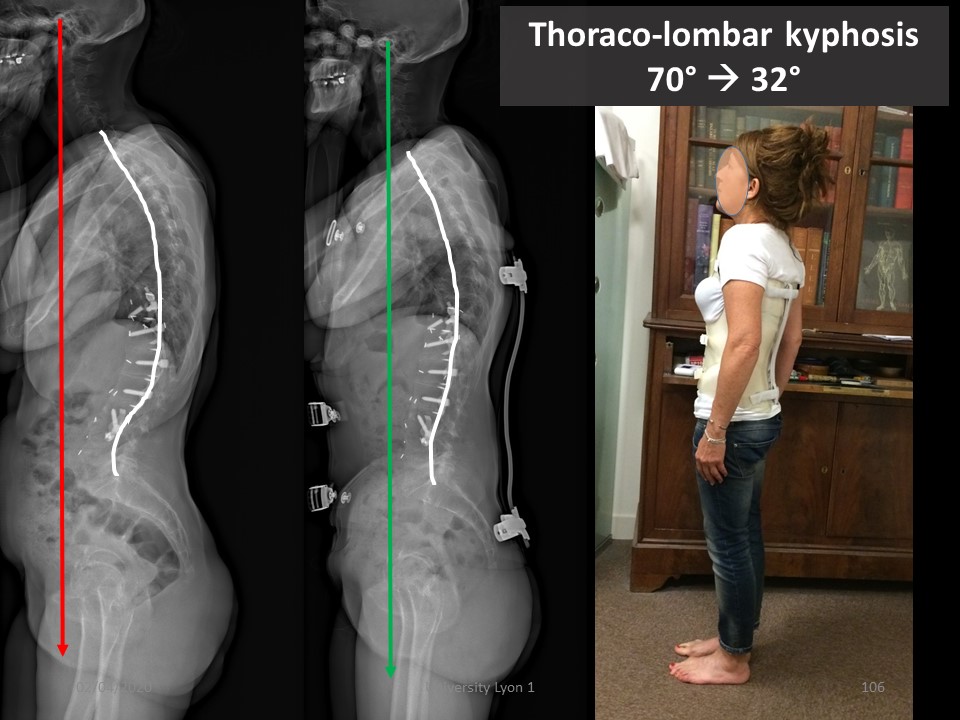
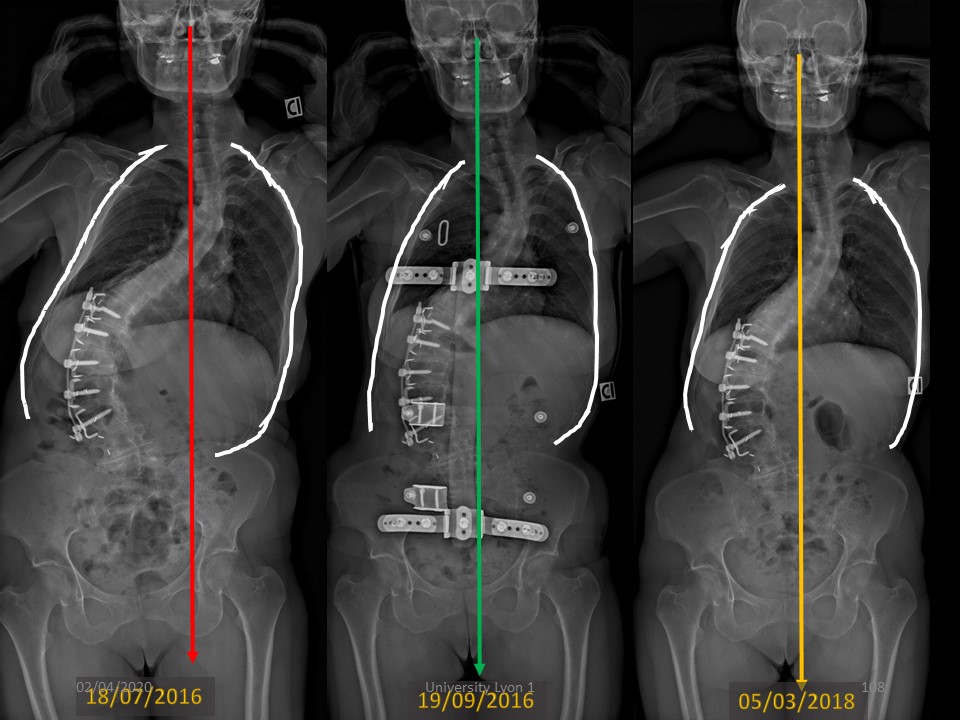
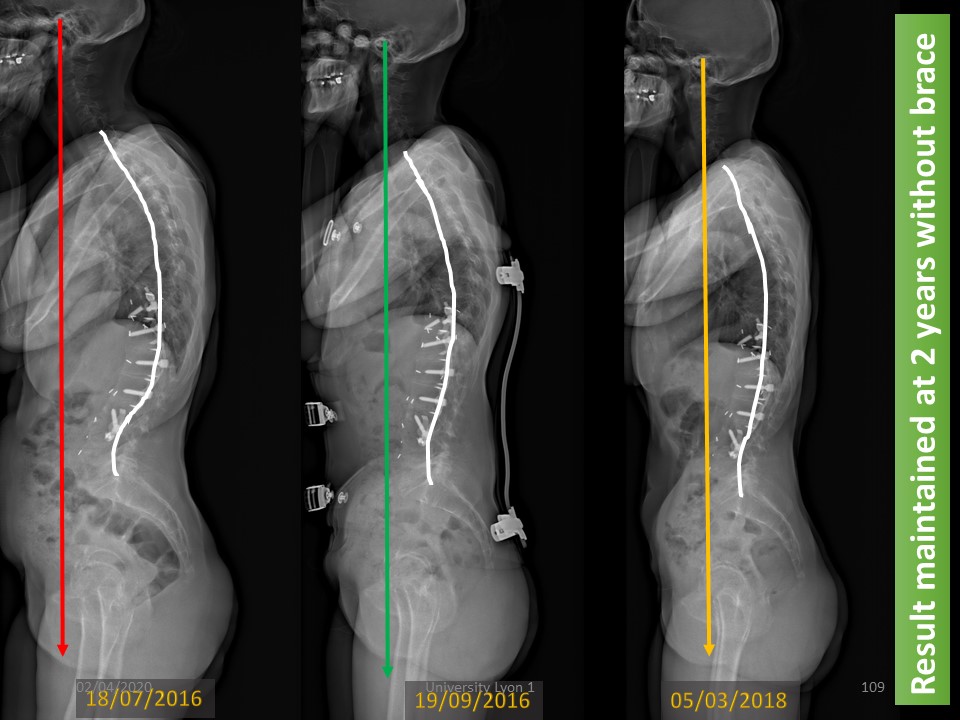
The Case n° 776 is an example of the new management. I see this patient at 60 years, 28 years after surgery with a good anterior Lumbar arthrodesis, but upper thoracic decompensation. The Frontal imbalance is 70 mm Right, Cobb angulation T9-L3 83° and Thoraco-lumbar kyphosis 70°. In the morning, she is very straight, then torsion appear during the day.
|
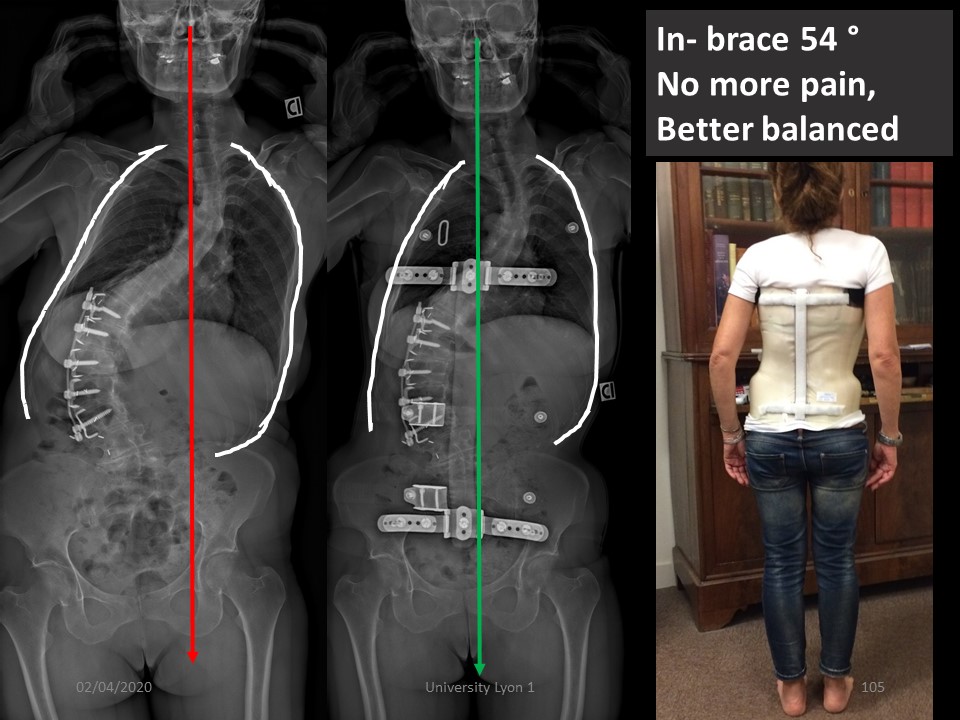 |
She did not want the recommended surgical revision and prefer to try bracing, In-brace Cobb angle was 54°, No more pain, and better balance.
|
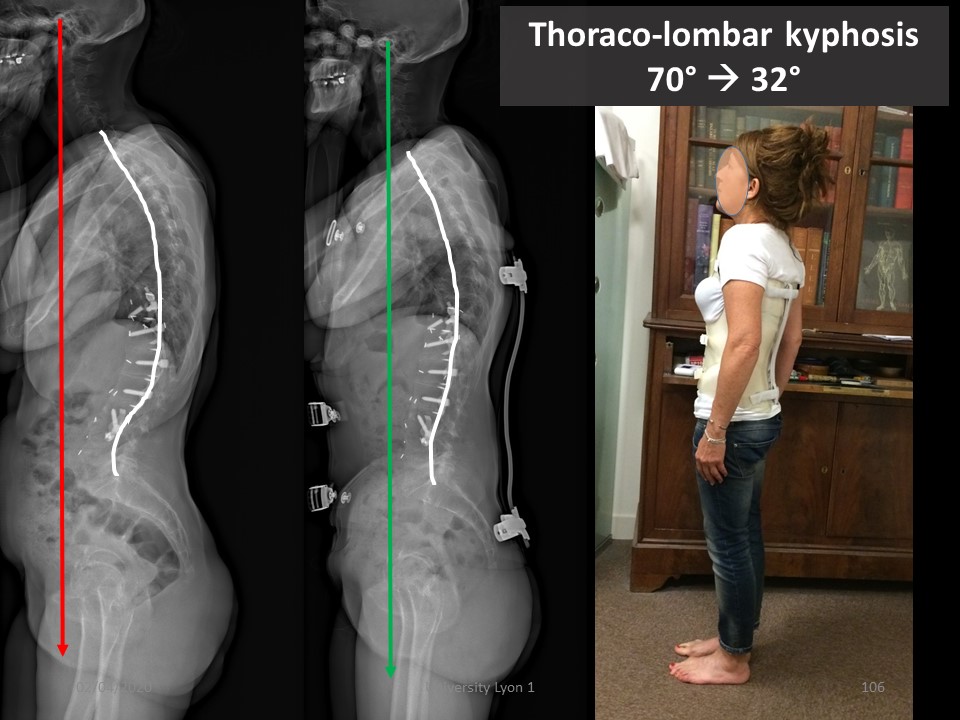 |
But the most spectacular result is in the sagittal plane with marked improvement in thoraco-lumbar kyphosis. Given the arthrodesis, this improvement is difficult to explain.
|
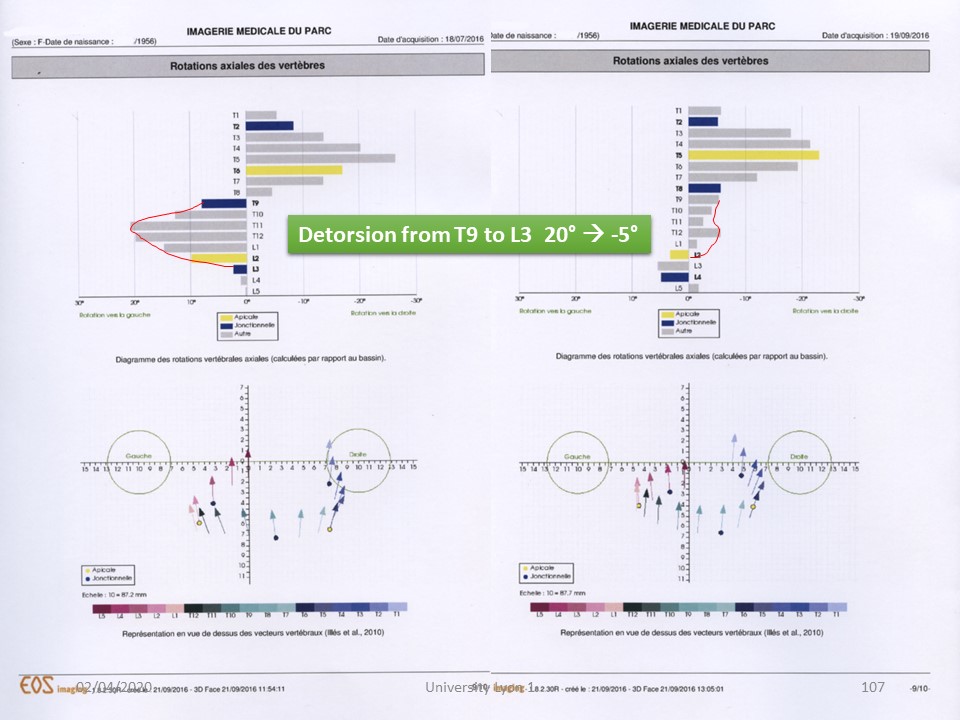 |
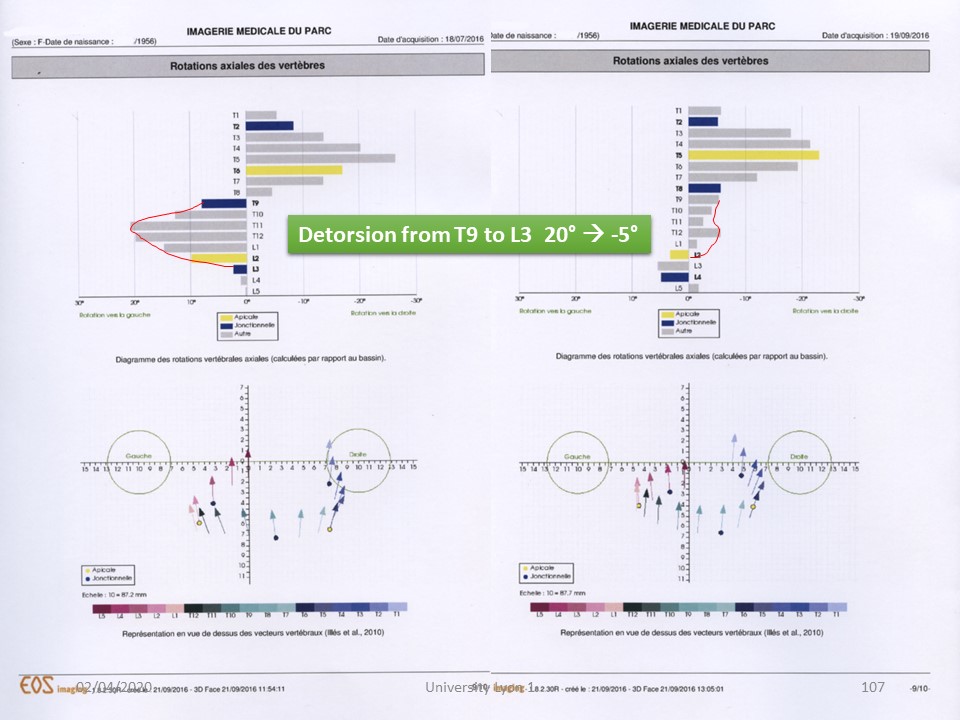
It is the EOS 3D study that shows the nearly 25° detorsion mechanism from T9 to L3, confirming that the ARTbrace is a detorsion brace, even in adults.
|
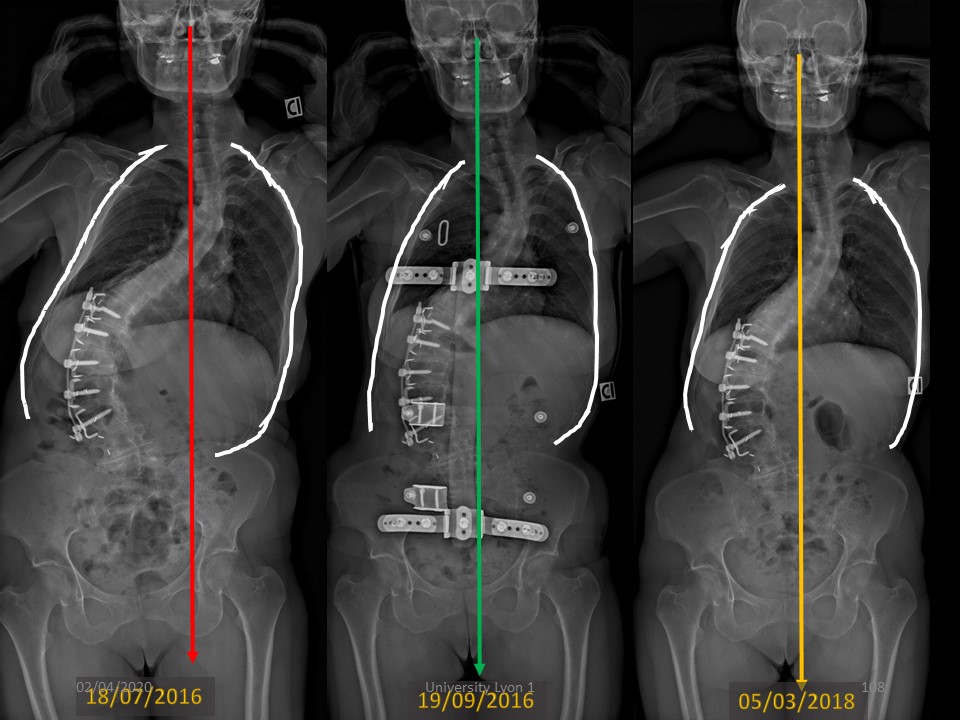 |
This improvement seems to be maintained over time here in the frontal plane,
|
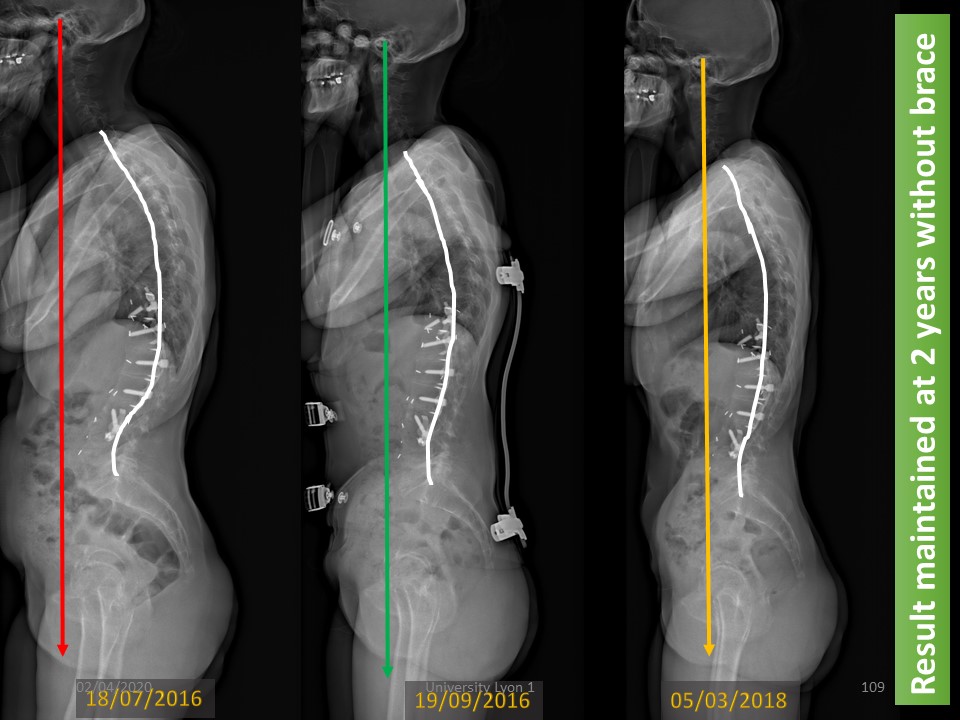 |
and the same in the sagittal plane. The improvement of thoraco-lumbar kyphosis is maintained without brace
|
 |
|
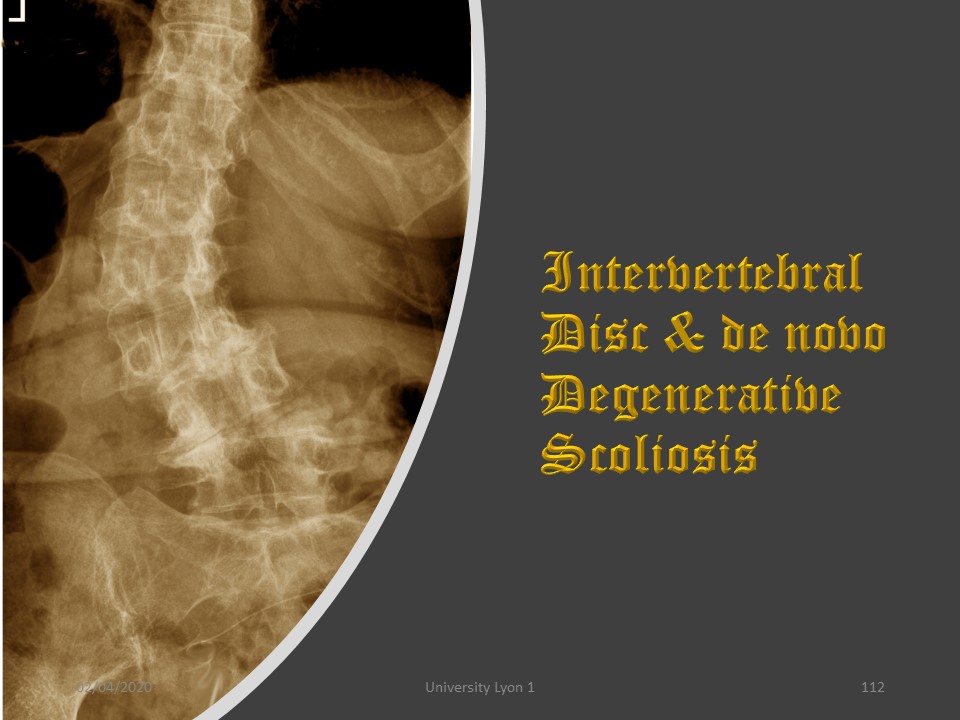 |
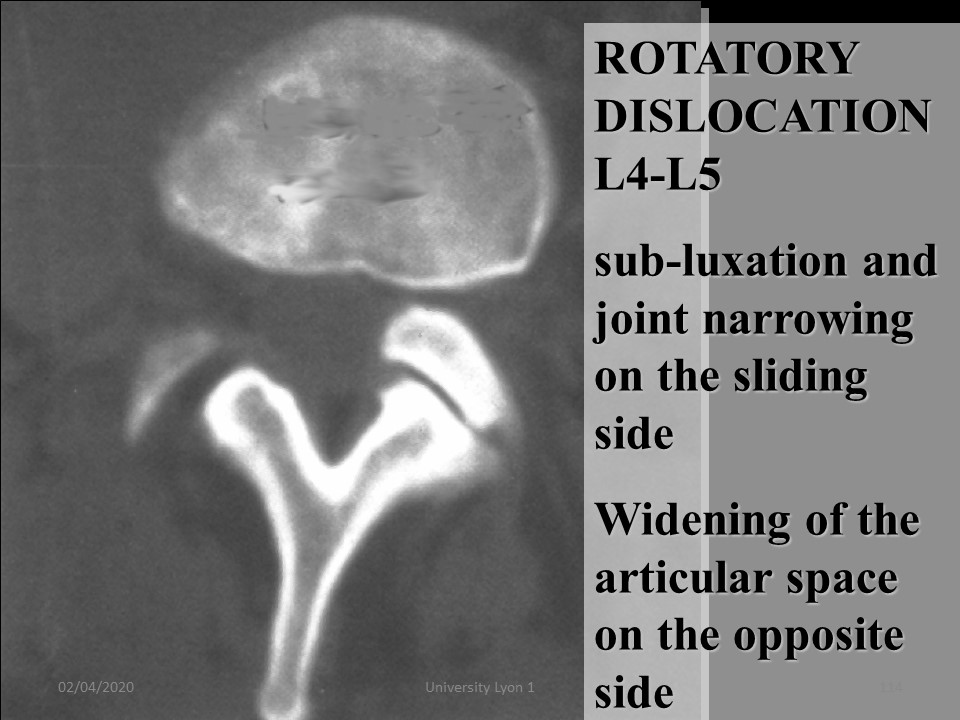
Discopathy is also the cause of so-called "de novo" scoliosis with rotary dislocation, here in L3-L4.
|
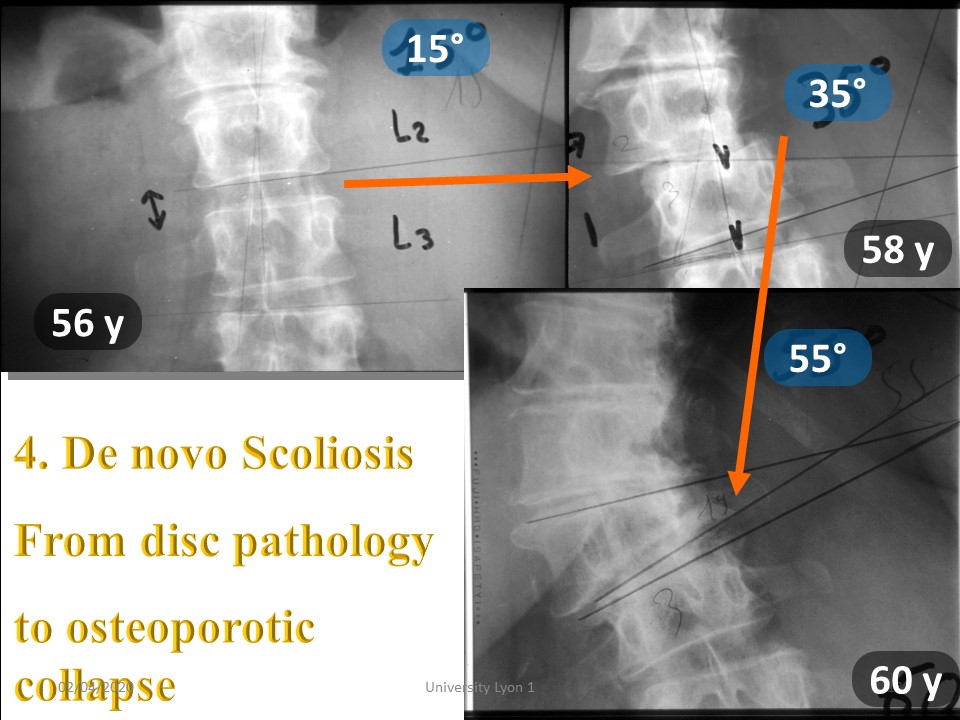 |
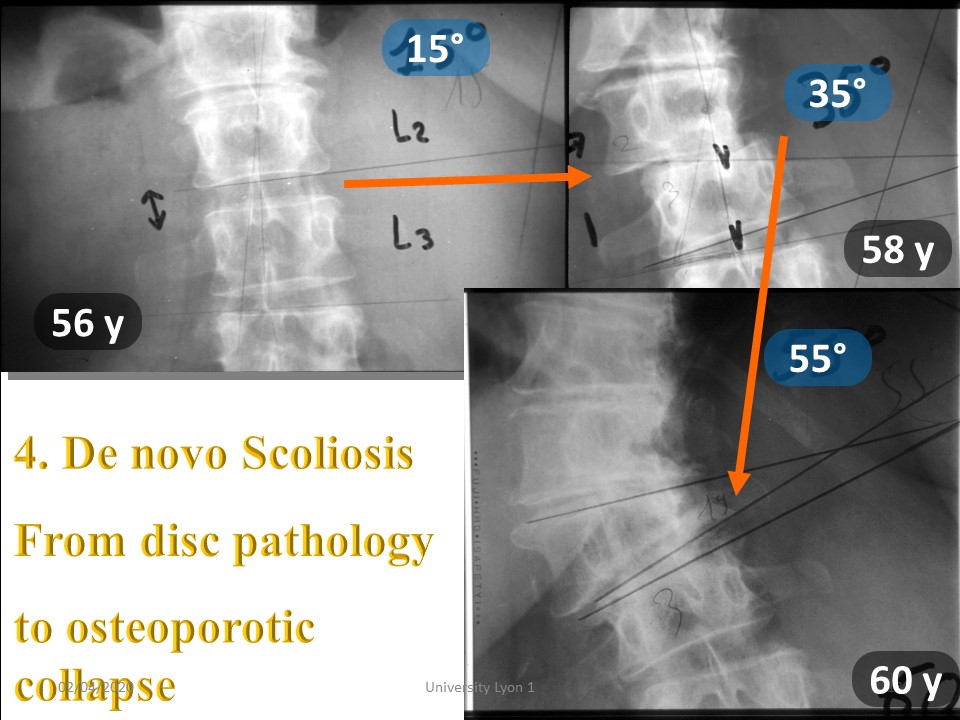
Here is a typical example of de novo scoliosis with late-onset and rapid evolution associating discopathy and probably osteoporosis. The progression of 40 ° is linear between 56 and 60 years.
|
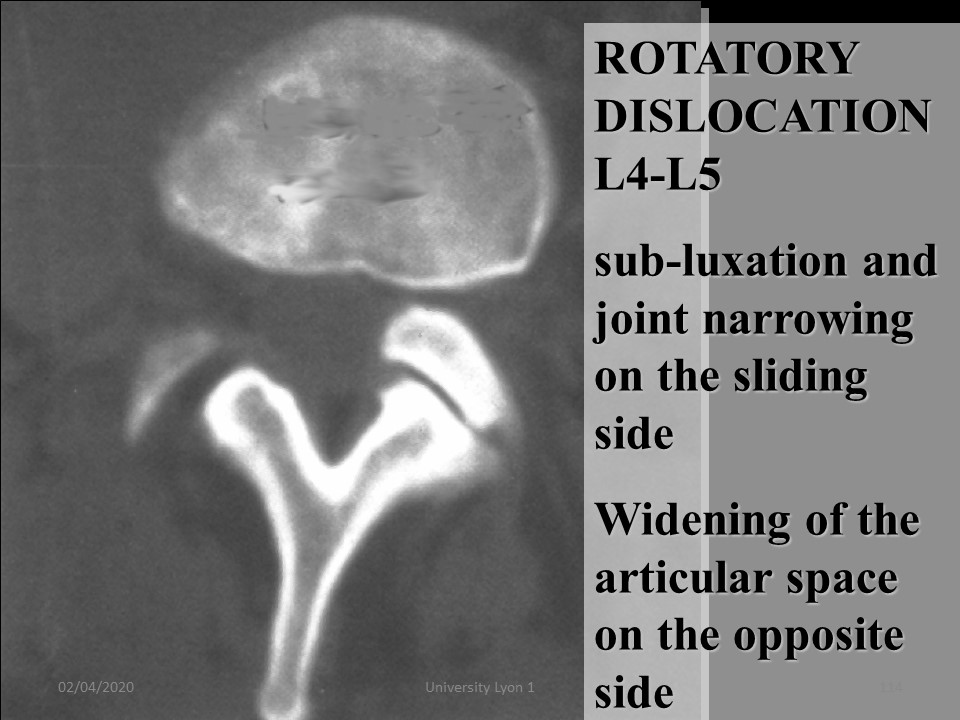 |
The usual mechanism is of intervertebral disc origin. It is the rotary dislocation visible on this cross section with. sub-luxation and joint narrowing on the sliding side, Widening of the articular space on the opposite side.
|
 |
|
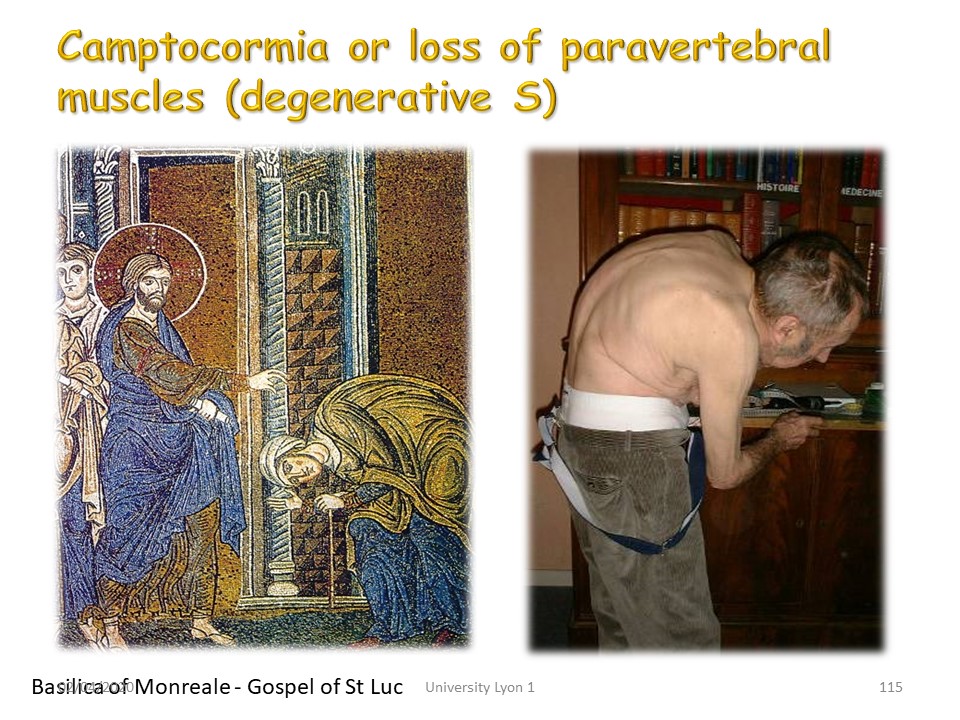 |
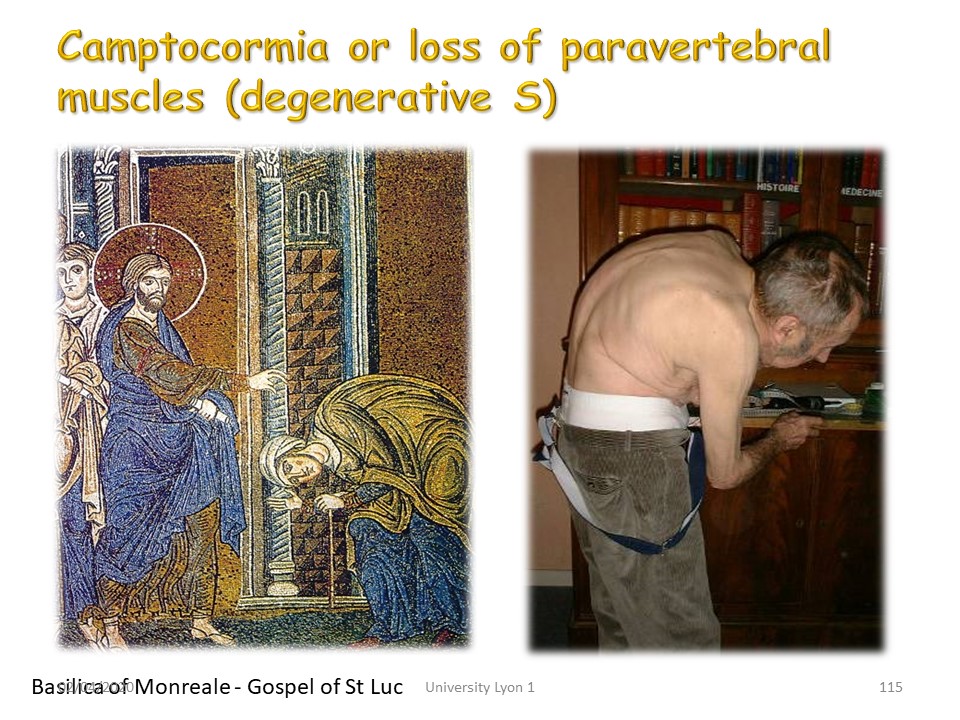
Camptocormia is linked to weakness of the deep posterior musculature. The patient increases kyphosis gradually to tighten his weak paravertebral muscles. There is often an extra-pyramidal context of Parkinson's disease. Some have mentioned paravertebral myopathy. The miraculous healing of such kyphosis is quoted in the Gospel of St. Luke and depicted on the mosaics of the Basilica of Montreale in Palermo.
|
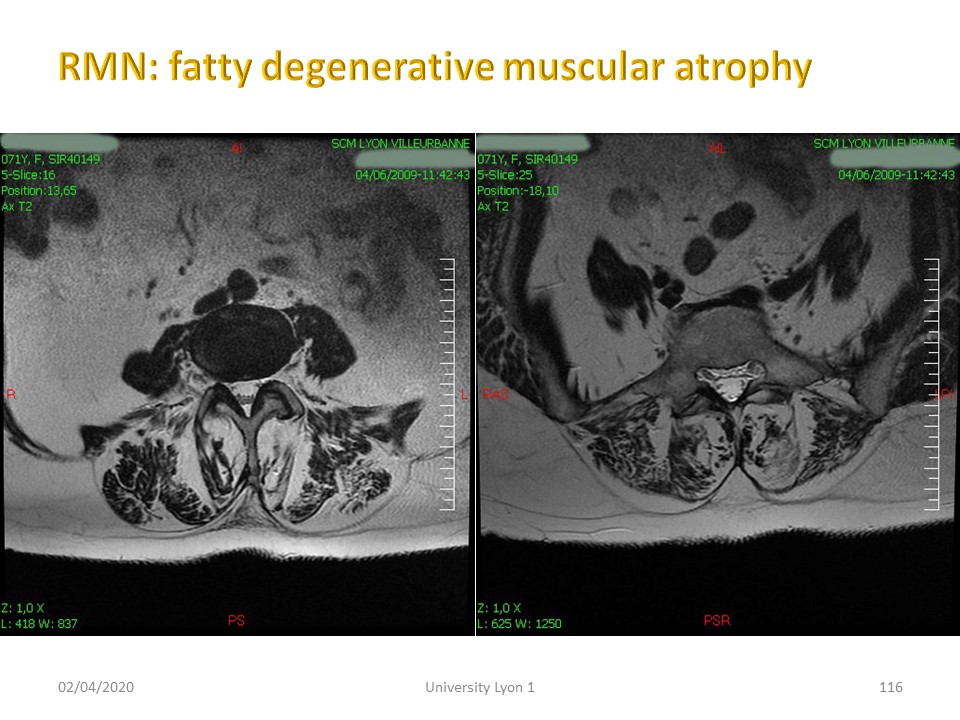 |
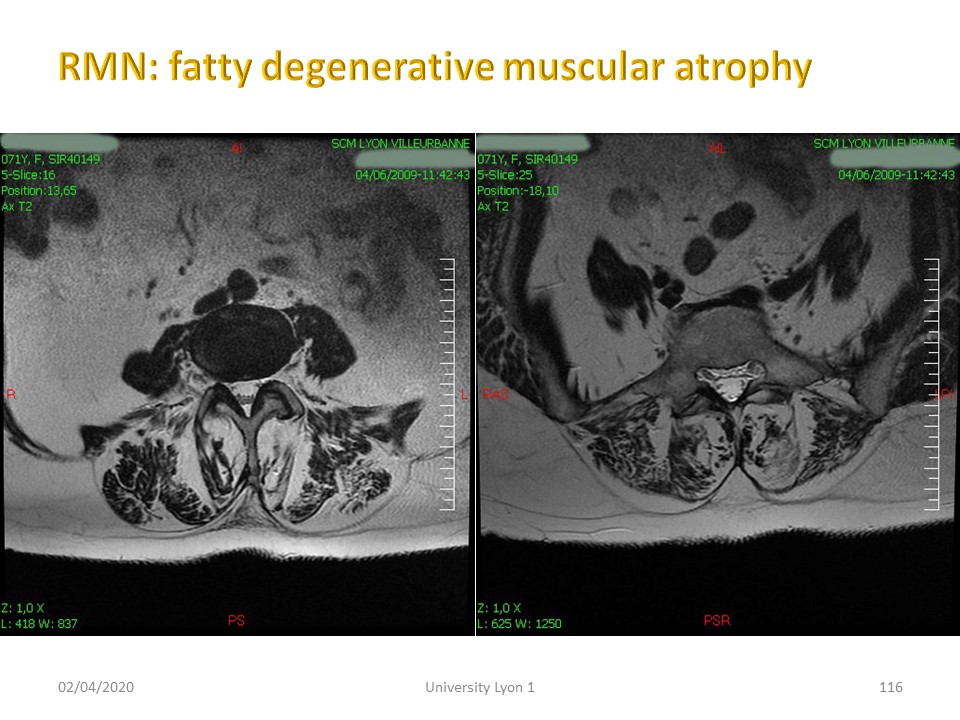
MRI cross sections highlight the fatty degeneration usually of extra-pyramidal origin with alteration of the reticulo-spinal system,
|
|
Comment in the certification part of the website
To view the full video presentation register for the certification course” www.scoliosisandspineonlinelearning.com
|
 |
|
 |

To register for Certification, please contact SSOL

|